Authors: Elizabeth Neiberg, JD and Kevin Obletz, JD, CVA

ORIGINALLY PUBLISHED BY THE AMERICAN ASSOCIATION OF PROVIDER COMPENSATION PROFESSIONALS
For decades, anesthesiology service lines have been predominantly provided by a combination of two types of providers: anesthesiologists and certified registered nurse anesthetists (“CRNA(s)”). By definition, anesthesiologists are physicians who have (i) completed medical school; (ii) at least one year of a clinical base year residency; and (iii) three years of residency in an anesthesia program. Alternatively, CRNAs are advanced practice nurses who have (i) earned a baccalaureate degree; (ii) practiced at least one year as an acute care nurse; and (iii) successfully completed a graduate-level nurse anesthetist program.[1]
The COVID-19 Pandemic forced America’s healthcare system into “crisis mode,” bringing to the forefront the issue of healthcare provider alternatives. Specifically, reliance on CRNAs can bridge the gap in healthcare settings that are facing physician shortages, while also decreasing the overall provider cost associated with anesthesia services. In light of hospital shutdowns and provider shortages, and with recognition that CRNAs can practice with the same effectiveness and safety of an anesthesiologist, the use of CRNA-only models should be given serious consideration, where allowable[2], especially considering that CRNAs are, in general, two to three times cheaper than anesthesiologists.[3]
To better understand the various interplay between anesthesiologists and CRNAs, it’s helpful to examine the spectrum of provider utilization, which will vary by state law. On one extreme, CRNAs provide and bill for anesthesia services independently. Certain states do not require CRNAs to be supervised at all by a physician, allowing them to practice to the full scope of their education, training, certification and licensure. At the other end of the spectrum, anesthesiologists may be the only providers administering and billing for anesthesia services in a particular setting. In between the two extremes, CRNAs provide anesthesia services under physician oversight, either medical direction or supervision. Under medical direction, an anesthesiologist directs from one to four CNRAs, and is present at specific stages of the anesthesia procedures. Under supervision, an anesthesiologist supervises four or more CRNAs at a healthcare facility, but is not required to be present during the actual anesthesia procedure. Some states that require physician supervision or direction do not require the physician to actually be an anesthesiologist. In other words, a physician with no expertise or experience in anesthesiology may be supervising or directing CRNAs simply due to their status as a physician.
A renowned 2010 simulation model first introduced the nation to the costs of various anesthesia delivery models. The subsequent report, also published in 2020 and titled “Cost Effectiveness Analysis of Anesthesia Providers”[4], has been repeatedly relied upon in scholarly journals and articles and is still referenced to this day. Most notably, the study indicated the following: (i) mortality among anesthesia had significantly decreased in the prior two decades, regardless of the provider; and (ii) during such time, the number of practicing CRNAs had also drastically increased. In 2018, the original 2010 simulation was re-visited, with parameters of the cost-effectiveness model updated to reflect the latest available data.[5] Not surprisingly, both the 2010 and 2018 simulations revealed that elimination of medical direction and supervisory delivery models and allowing CRNAs to practice to the full extent of their training, substantially reduces costs associated with anesthesia delivery. The 2018 simulation looked at various settings (e.g., inpatient, outpatient and ambulatory surgery centers) as well as various anesthesiology demands, comparing average demands across the board. While revenue and costs differ across settings, under all scenarios, revenue was found to be identical between anesthesiologists and CRNAs, while costs for anesthesiologists were at least double that of CRNAs. The simulation unilaterally concluded that, while not always feasible, CRNAs acting independently is undoubtedly the least costly per procedure while also producing the greatest net revenue.
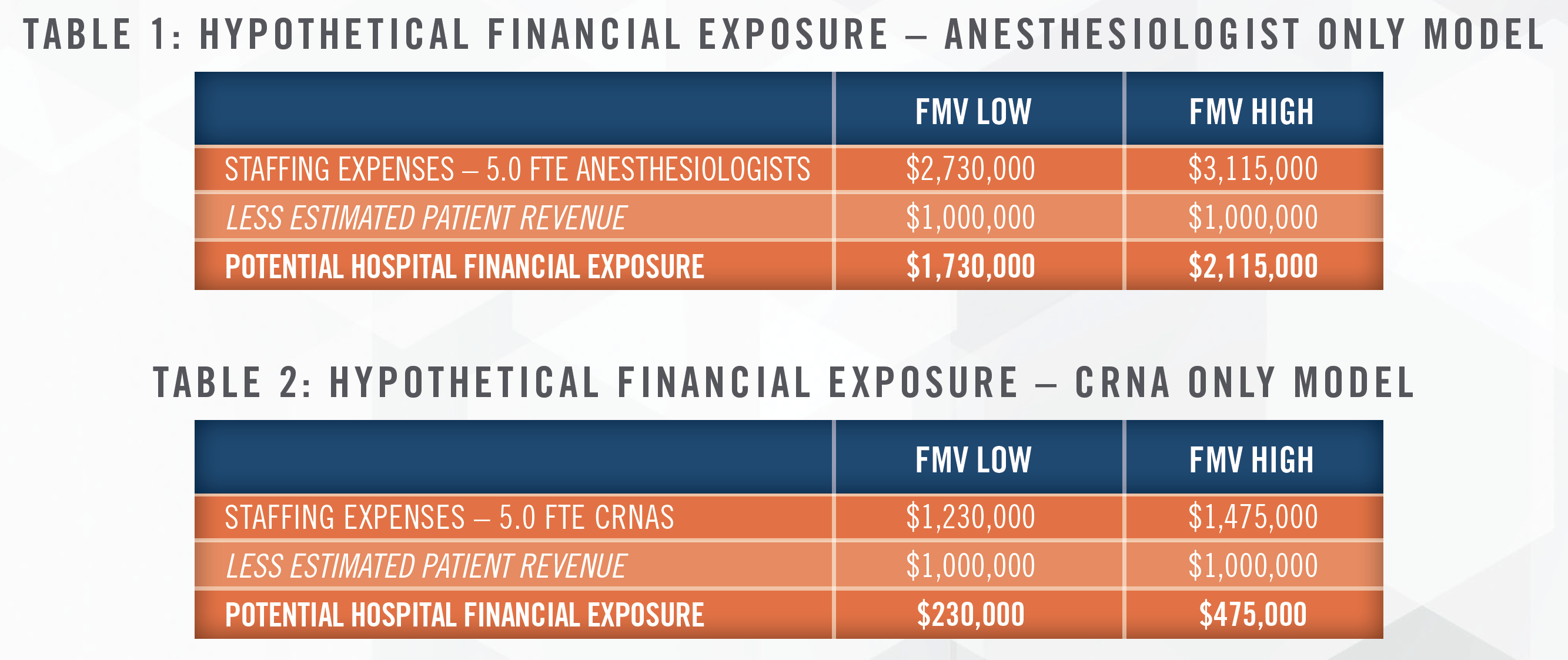
To demonstrate the cost effectiveness of CRNA deployment, valuation of hypothetical anesthesia services arrangements were performed based upon utilization of provider compensation and production “Surveys.” Based on current Survey data, the fair market value (“FMV”) cost for a 1.0 full-time equivalent (“FTE”) independent contractor anesthesiologist reasonably ranges from $546,000 to $623,000 per year, inclusive of cash compensation, benefits and taxes, whereas the FMV cost for a 1.0 FTE independent contractor CRNA reasonably ranges from $246,000 to $295,000 per year, inclusive of cash compensation, benefits and taxes.[6] Therefore, assuming patient revenue remains steady regardless of the staffing model utilized, as described above, the following table demonstrates a hospital’s potential financial exposure based on the utilization of 5.0 FTE anesthesiologists versus 5.0 FTE CRNAs:
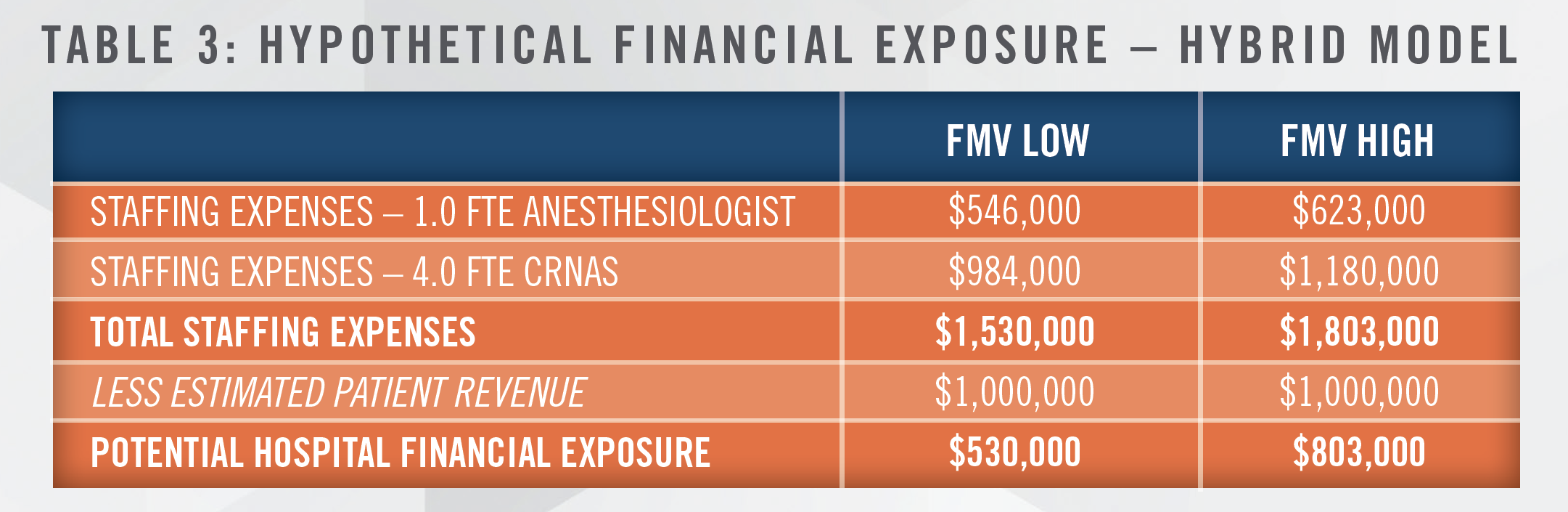
Furthermore, a medical direction and/or supervision model whereby one FTE anesthesiologist supervises/ directs four FTE CRNAs yields the following result:
Although state law may limit the extent of CRNA utilization, research and practical application of data suggests that the potential for cost savings in staffing an anesthesia service line increases as CRNA utilization increases. With the prevalence of physician staffing shortages and as hospital budgets continue to get squeezed, now is the time for health systems to re-evaluate their anesthesia delivery model to ensure optimization of cost savings. Where allowable, this may mean it’s time to give serious consideration to the CRNA-only model.
[1] While a third provider-type, anesthesia assistants (“AA(s)”), also provide anesthesia services, AAs are always assistants to an anesthesiologist, and are prohibited from providing services unsupervised/directly.
[2] Anesthesiologists in the United States are licensed to practice independently in all 50 states plus Washington D.C., whereas CRNAs may not be able to practice independently, subject to state law requirements.
[3] Hogan, P. Seifert, R. Moore, C. Simonson, B. (2010). Cost effectiveness analysis of anesthesia providers. Nurs Econ. 2010 May-Jun; 28(3): 159–169.
[4] Hogan, P. Seifert, R. Moore, C. Simonson, B. (2010). Cost effectiveness analysis of anesthesia providers. Nurs Econ. 2010 May-Jun; 28(3): 159–169.
[5] Cintina, I., Hogan P., Schroeder, C., Simonson, B., Quraishi, J., Cost Effectiveness of Anesthesia Providers and Implications of Scope of Practice in a Medicare Population. Nursing Economics. March – April 2018, Volume 36, No. 2.
[6] Utilizing data reported at the median to establish the low end of the FMV compensation range for both anesthesiologists and CRNAs, and (i) for anesthesiologists, data reported at the 75th percentile to establish the high end of the FMV compensation range; and (ii) for CRNAs, data reported at the 90th percentile to establish the high end of the FMV compensation range.
