Authors: Luis A. Argueso and Andrew L. Worthington

![]() FORECASTING CHANGES TO MEDICARE REIMBURSEMENT
FORECASTING CHANGES TO MEDICARE REIMBURSEMENT
Hospitals and health systems frequently enter into hospital-based clinical coverage arrangements (“HBCCAs”) with independent practices to cover their hospital-based service lines (e.g., anesthesiology, emergency medicine, hospitalist medicine, intensive care, and radiology). Because hospital-based providers commonly generate lower collections from their professional services than their costs to provide those services, HBCCAs usually involve some form of financial support from the hospital. Specifically, the level of financial support paid by a hospital under an HBCCA is going to be directly related to the level of professional collections generated by the contracted medical group. The more professional collections generated, the less financial support provided by the hospital.
HealthCare Appraisers recently published a comprehensive analysis and summary of the 2021 Medicare Physician Fee Schedule (“MPFS”) final rule. This article focused largely on the rebasing of work relative value units (wRVUs) and how this will affect physician employers using compensation-to-Work-RVU models. As discussed in the article, the base wRVUs for evaluation and management care increased. However, these adjustments solely apply to wRVUs and clinical care in an outpatient setting. The wRVUs for evaluation and management care provided in a hospital-based setting have not been adjusted.
In early December, when the 2021 Final Rule proposals were first made available, it became quickly apparent that HBCCAs were going to be greatly affected. Initially, it was projected that certain specialties, including anesthesiology, critical care, emergency medicine, hospitalist medicine, and radiology were all going to see material decreases to Medicare reimbursement. However, as of December 27th, 2020, this is no longer the case.
![]()
![]()
![]()
![]()
On December 27th, 2020, Medicare updated the MPFS conversion factor to $34.89 as a part of the Consolidated Appropriations Act. This is an increase from the initial projection of $32.40 from early December. However, the new conversion factor is still around 3% lower than the $36 conversion factor for 2020. For HBCCAs, the level of professional collections is vital in determining appropriate levels of compensation (and for that matter, fair market value compensation). We anticipate that Medicare revenue for providers covering hospitals pursuant to HBCCAs will decrease by nearly 3%, the full amount of the decrease in the MPFS conversion factor. The observation holds for anesthesiology providers as well, as their conversion factor was decreased from $22.20 to $21.56. While the decrease is diminished relative to the original rule finalized prior to the Consolidated Appropriations Act, it is important to note that Medicare reimbursement decreases will have a material impact to hospital-based providers given the high proportion of Medicare (and other government payors) in their payor mix. The exceptions to this observation are emergency medicine and laborist practices. Both specialties benefited from increases in wRVUs for their commonly-used CPT codes, which is expected to result in reimbursement increases of 2% and 7% for emergency medicine and laborist physicians, respectively.
![]()
![]()
![]()
![]()
As discussed above, the reimbursement landscape for physician groups has taken a turn for the better relative to the initial final rule. Hospitals and health systems need to be diligent when handling re-negotiation requests from their contracted providers. All things equal, anesthesiology, hospitalist, intensive care, and radiology groups could experience a decrease in their aggregate level of collections. In contrast, emergency medicine and laborist providers could experience increased professional collections. However, these specialties will all continue to have patients who are uninsured or insured by Medicaid, commercial, and other government patients. The Medicare reimbursement is only one piece of the puzzle.
As part of our fair market value services, we offer value-added analyses that can help provide actionable insights when negotiating the terms of HBCCAs. Below, is a summary of standard collections estimate process included as part of all opinions involving HBCCAs:
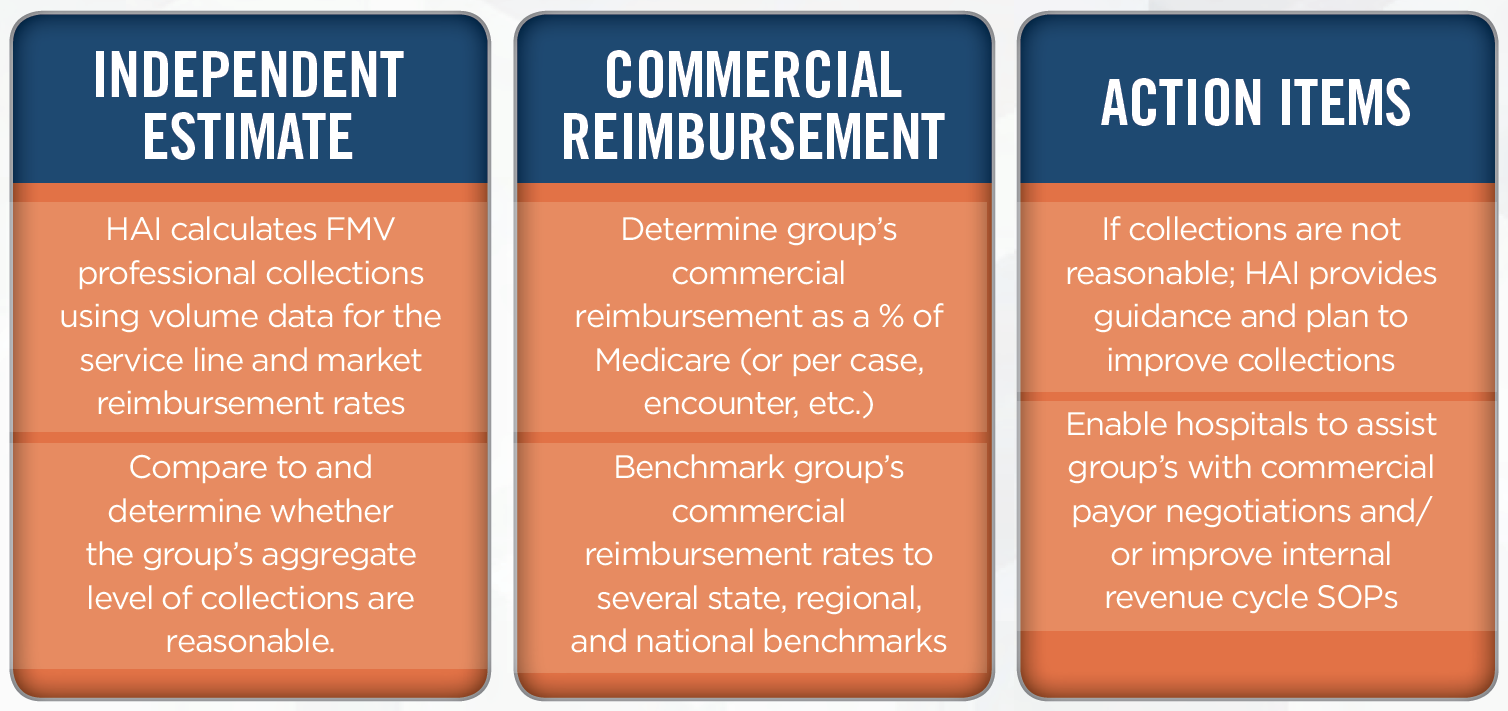
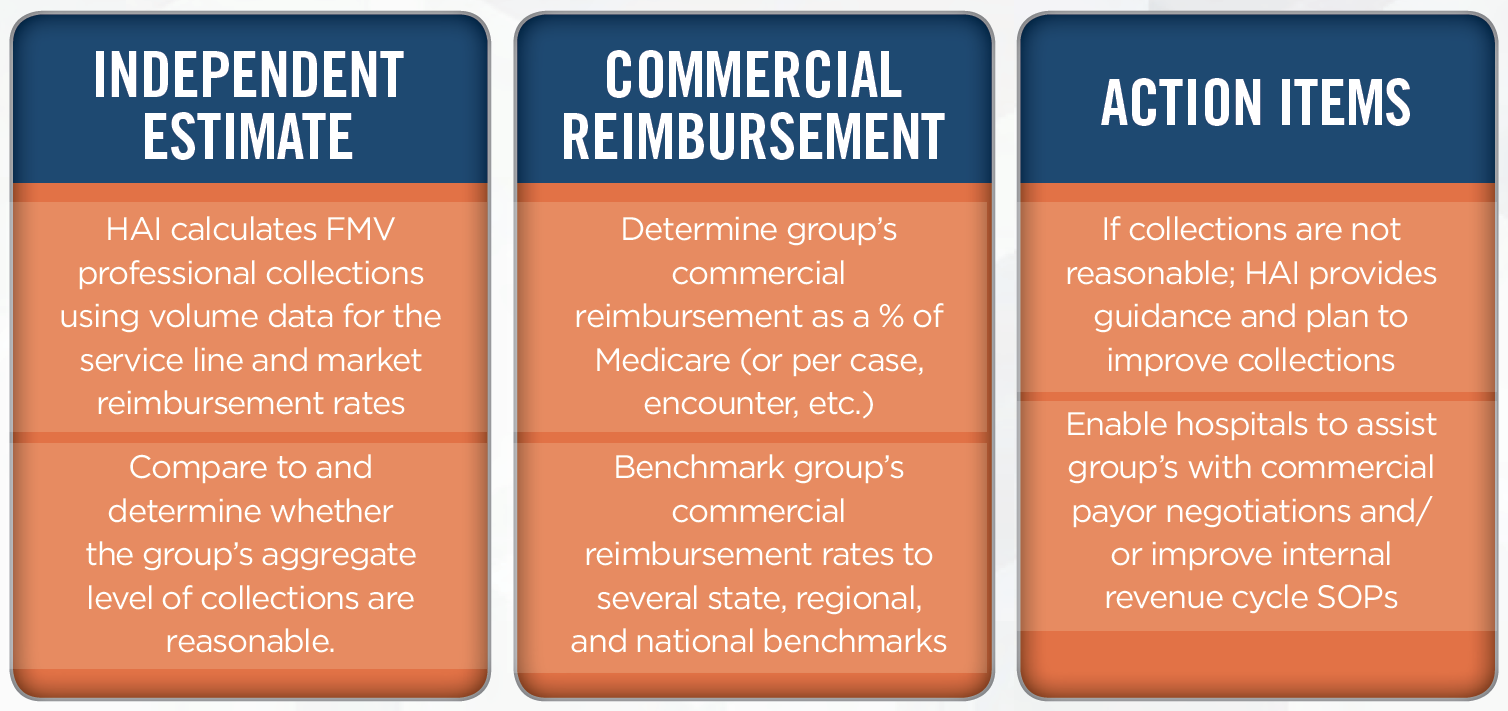
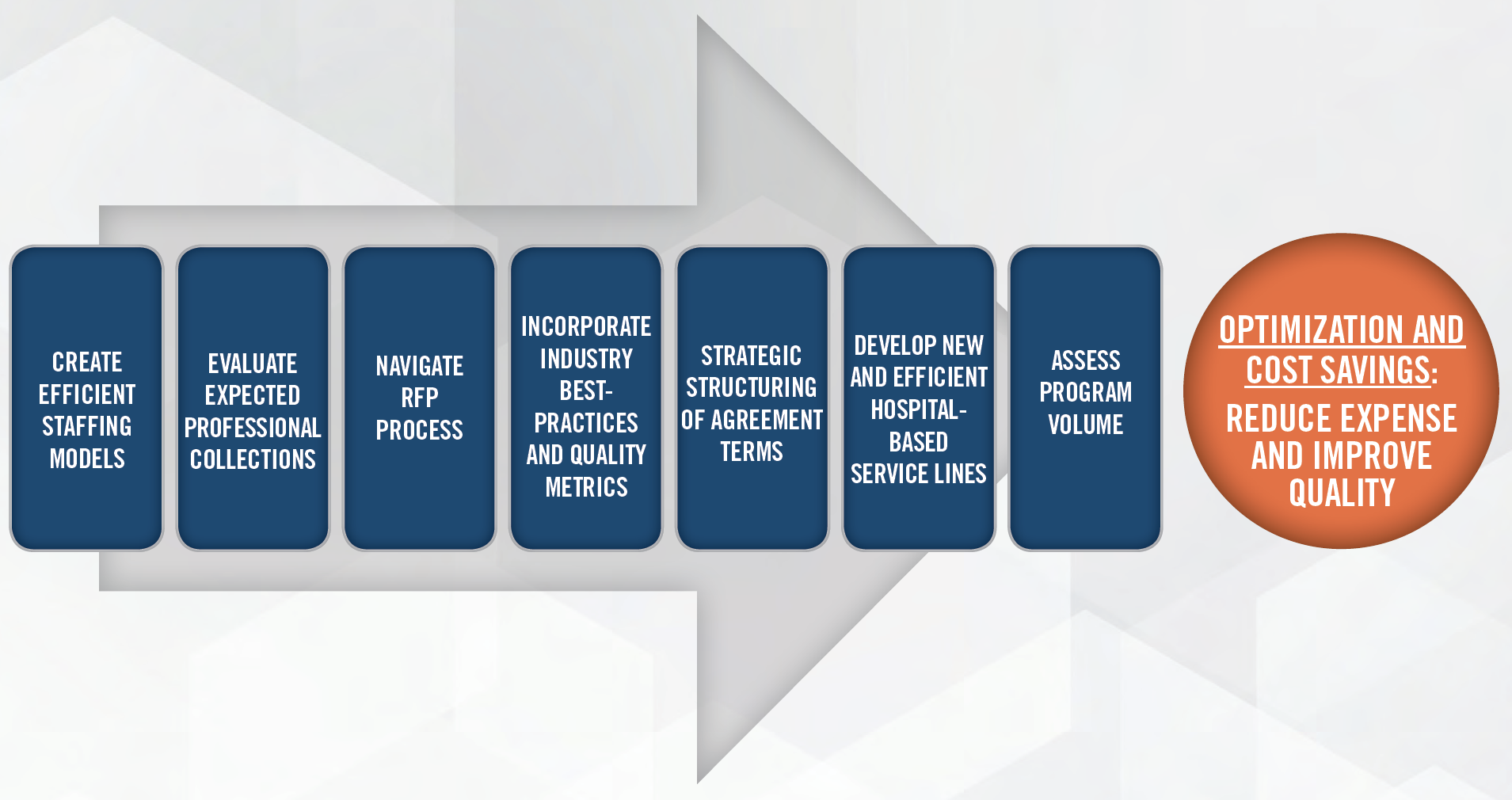
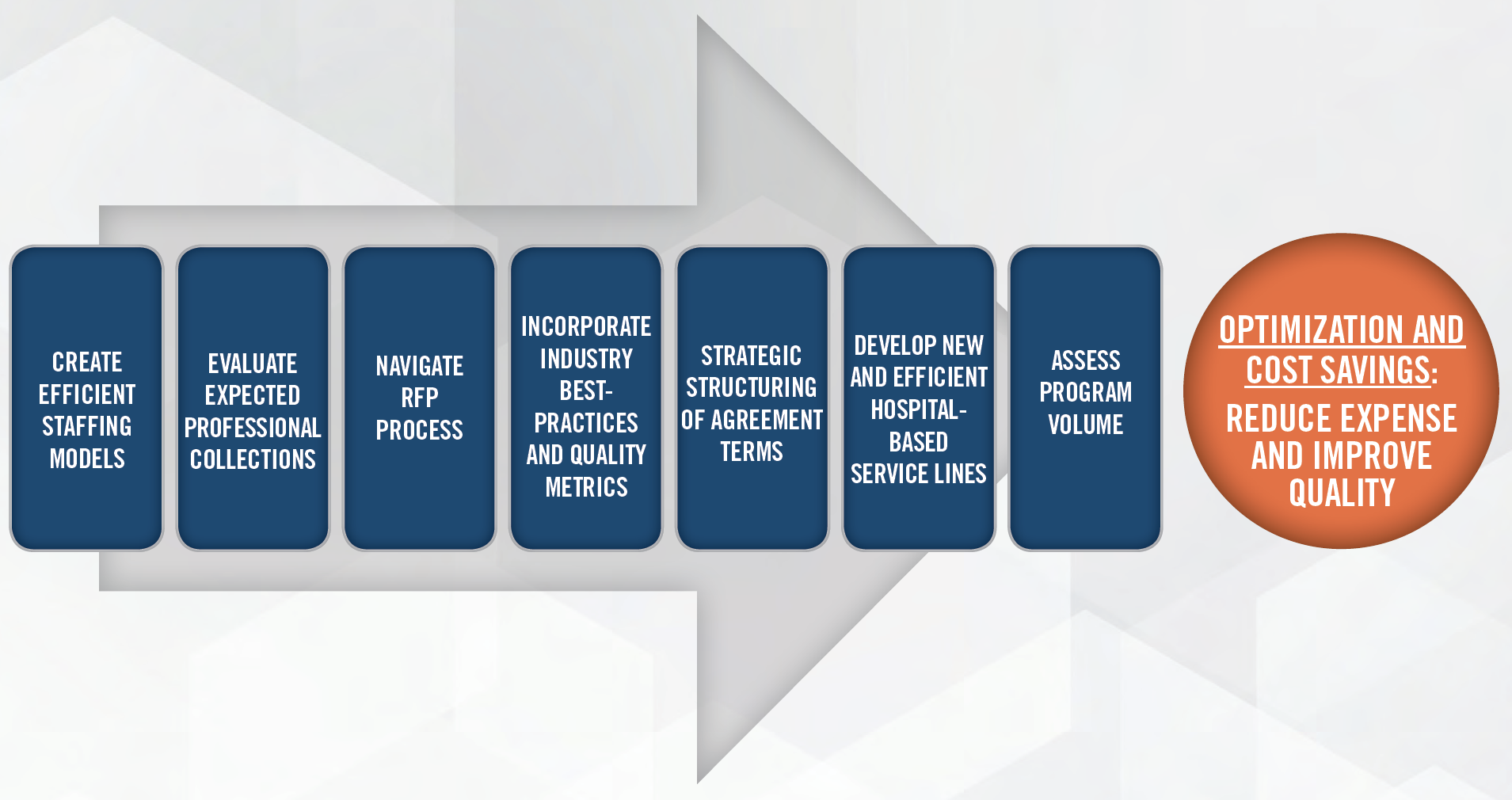
Regardless of the specialty or service line, HealthCare Appraisers can assist with estimating and benchmarking professional collections under an HBCCA. We take a holistic approach that also considers the coverage and type of care being provided. We can assist with assessing collections, negotiating with provider groups, with the ultimate goal being cost savings and service line optimization.
You may also be interested in reading our 2021 Review & Benchmarking Guide: Trends and Data Insights for Hospital-Based Clinical Coverage Arrangements.
