Author: Jake Bitting, Fred Lara, CFA, ASA, CVA, and Hunter A. Wolfel

On October 13, 2023 the Governor of California signed the California Senate Bill No. 525 (“SB525”) into law, which is expected to raise the minimum wage for many California healthcare workers (W2 employees and 1099 independent contractors) from $16.00 per hour to $25.00 per hour according to a preset escalation timeline, beginning June 1, 2024. On January 10, 2024, Governor Gavin Newsom indicated that he is seeking changes to the law which will primarily be focused on further considering the state budget conditions and revenues. While the actual implementation of SB525 could be delayed depending on California’s financial position, it is still expected that the law will take effect at some point in the future. We provide commentary herein about the background of the law as it stands currently, and its potential impacts on both healthcare services organizations and the valuation of certain healthcare transactions.
Notably, (i) the scope of the term “healthcare worker” within the law includes not only those providing direct patient care but also anyone who supports the delivery of healthcare (e.g., technicians, call center workers, food service workers, janitorial staff, billing personnel, etc.), and (ii) the impact of the law, including the time to reach $25.00 per hour, will vary based on the healthcare facility type and/or location (“Facility Category Designation”).
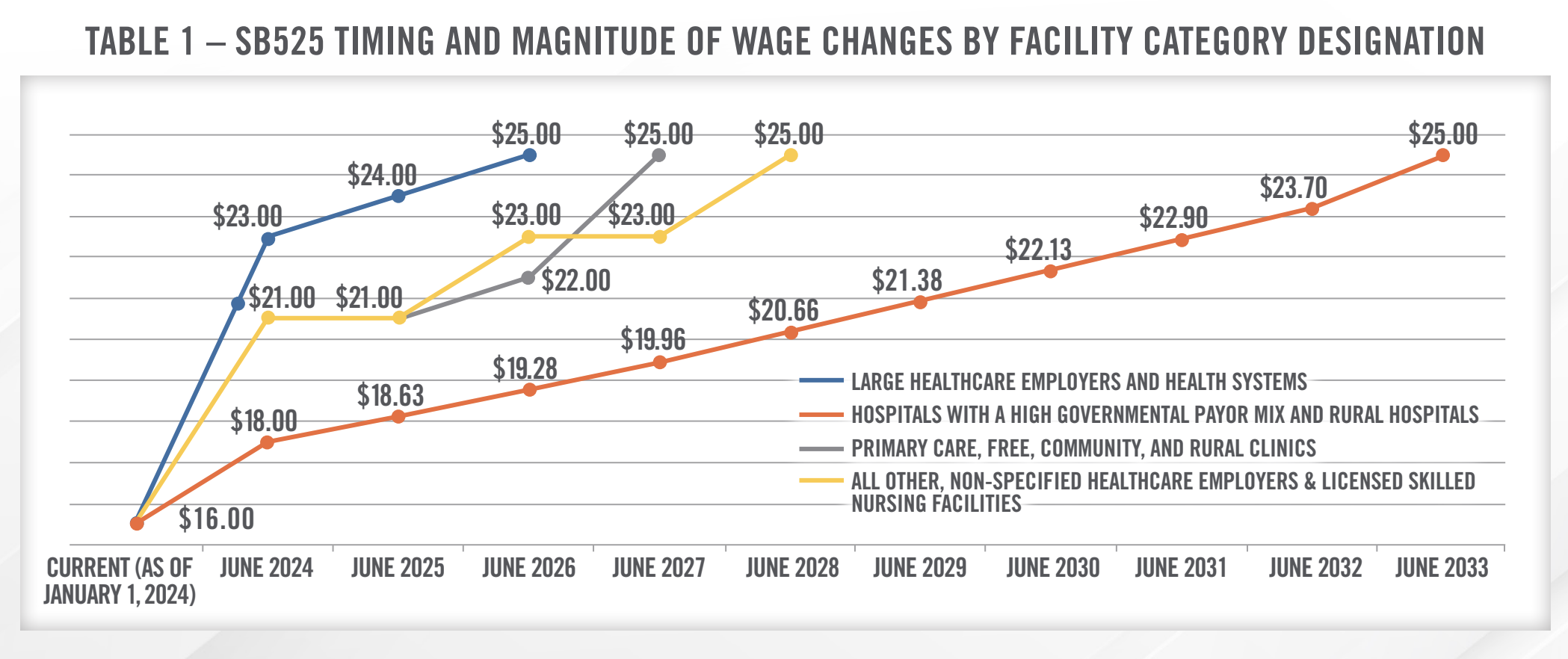
Such Facility Category Designation will set the timing and magnitude of wage increases. The full impact of the minimum wage increase extends over a longer period (i.e., 9 years) for smaller, more financially disadvantaged health care facilities, while requiring only two years to reach its full impact for larger healthcare employers and health systems. Table 1 below summarizes the specific timing of he wage changes by facility category designation.
One source[1] (the “Study”) estimates that over 469,000 workers will be affected by the wage increase, including over 50,000 workers who currently earn slightly above $25.00 per hour but might receive a pay increase to maintain their pay premium. The Study further asserts that affected workers will receive an average wage increase of over $5.74 per hour, or about a 30% increase. Considering the composition of the workforces in the healthcare marketplace, the impacts of the wage increases are expected to vary by facility type.
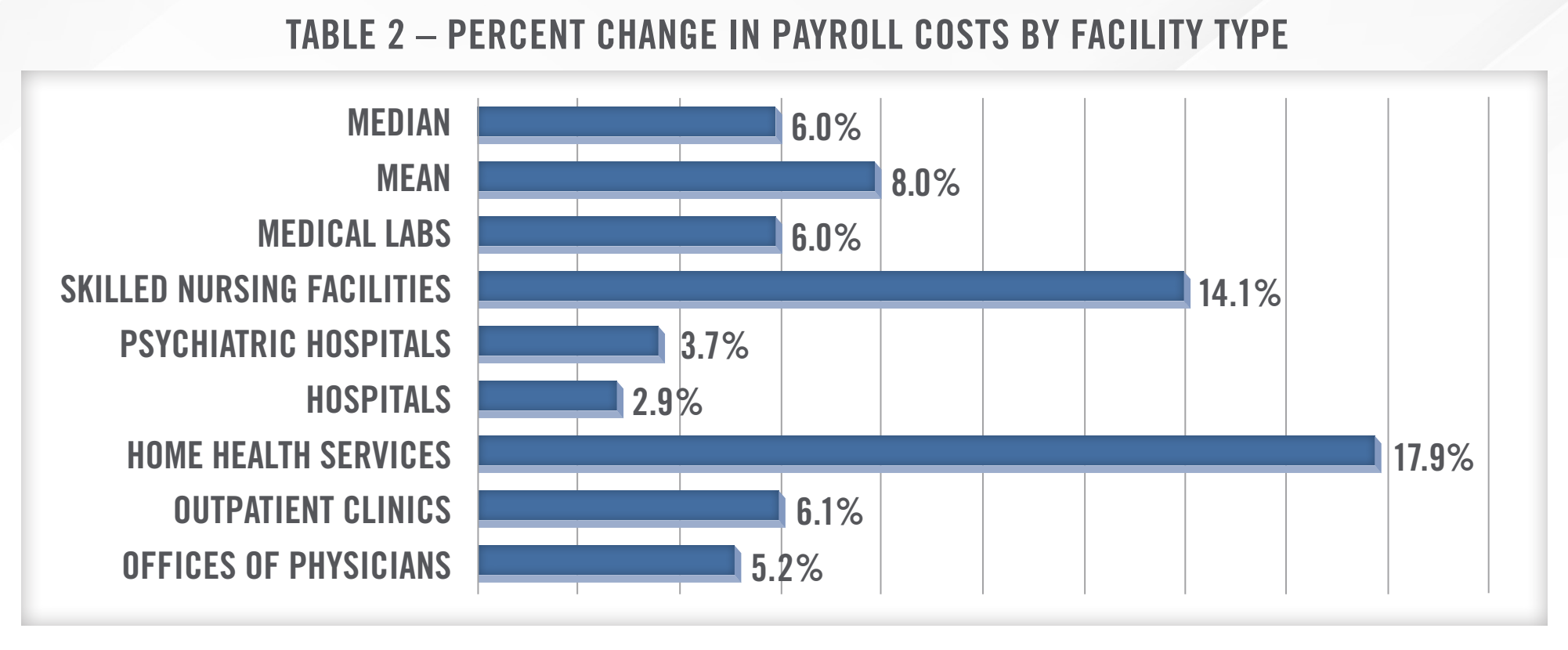
The above chart, based upon data from the Study, demonstrates that home health services and skilled nursing facilities are expected to see the greatest increases in operating costs, likely as a result of their having (i) the largest proportion of workers receiving a pay raise, (ii) a higher average wage increase per affected worker, and (iii) the largest percentage of labor costs as a percent of total operating expenses. This stands in contrast to physician offices, outpatient clinics, and hospitals, which, per the Study, are not expected to experience as great of an impact to their operating costs.
Although the primary focus of SB525’s impact is hourly workers, it also impacts salaried employees. Specifically, the law provides that salaried employees should receive the greater of (i) 150% of the applicable health care worker minimum wage, or (ii) 200% of the generally applicable state minimum wage. The inclusion of salaried employees will eliminate the ability of health care companies to transition hourly employees to salaried employees to counteract the forthcoming cash compensation increases.
Lastly, we note that SB525 extends the definition of healthcare workers to include independent contractors. Independent contractor healthcare workers are covered if there is a contract with the health care facility to provide health care services or services supporting the provision of health care, and the health care facility directly or indirectly exercises control over the contractors’ wages, hours, or working conditions. As a result of this provision, the natural market reaction to outsource in order to avoid the regulation is mitigated.
![]() IMPACTS TO OPERATIONS TEAMS AND VALUATIONS
IMPACTS TO OPERATIONS TEAMS AND VALUATIONS
As SB525 takes effect, HealthCare Appraisers will be considering the implications of the law within our Fair Market Value analyses. While we cannot fully predict the market’s reaction to these changes, it will be no surprise if there are unintended consequences to SB525 as non-governmental market participants take action to offset the profit margin impact of the regulations. These changes may include cost containment measures such as layoffs or further incorporation of technology-based business solutions, as well as revenue enhancement measures such as aggressive payor rate negotiations or lobbying for increased Medi-Cal reimbursement and/or increased GPCI adjustments to practice expense relative value units.
What we can predict with more certainty is the analyses types likely to be most impacted – specifically, those that include a meaningful amount of minimum wage workers affected most by SB525. These may include, but are not limited to, management agreements, revenue cycle management services, staff leasing, ambulance transport, transcription services, skilled nursing facility, and home health valuations. Depending on the relationship of the contracting entities, opportunities may exist for cross-referrals, which would, therefore, require that compensation fit within the lower and upper limits of FMV, as opposed to not exceeding the FMV upper limits. Implementation of SB525 would serve as a de facto “floor” of FMV, which may differ from the FMV lower limit that might otherwise have been established.
HealthCare Appraisers does not provide legal advice and would encourage operators to consult an attorney regarding the legal ramifications of SB525. However, please reach out to HealthCare Appraisers for assistance with navigating the implications of SB525 or any of its future amendments.
CONTACT THE EXPERTS AT HEALTHCARE APPRAISERS TO DISCUSS YOUR ADVISORY AND VALUATION NEEDS REGARDING THE IMPACT OF CALIFORNIA’S HEALTHCARE MINIMUM WAGE LAW ON VALUATIONS.
