Authors: Tammy Truong and Alyse Bentz, JD, MPH

Originally published by the American Association of Provider Compensation Professionals.
The United States is predicted to be imminently faced with a physician shortage, with a report from the Association of American Medical Colleges (“AAMC”) projecting a shortage of up to 139,000 physicians by 2033.[1] This shortage is likely to spotlight the use of Nurse Practitioners (“NPs”) and Physician Associates (“PAs”) by health systems and practices to ensure appropriate staffing levels and adequate clinical coverage.[2] In consideration of this anticipated shift in care delivery, this article explores some of the key differences between NPs and PAs.
![]() EDUCATION AND OTHER DIFFERENCES
EDUCATION AND OTHER DIFFERENCES
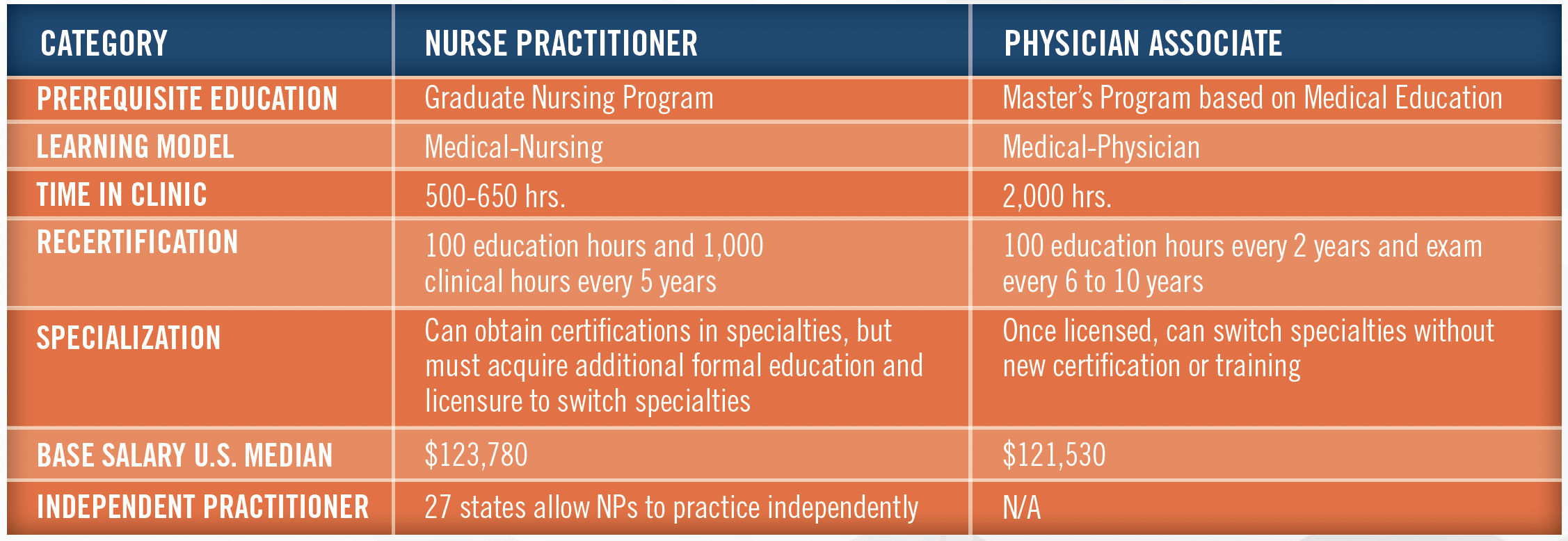
While both NPs and PAs are projected to be in demand due to the impending physician shortage, the required education and continuing learning requirements may impact the extent to which the healthcare gap is fulfilled by NPs versus PAs. Additionally, educational costs and return on investment may also impact the decision making for program applicants. See the below table for a comparison of the educational requirements, base salaries, and scope of allowed practice between NPs and PAs.[3]
![]() DISCUSSION OF QUALITY OF CARE
DISCUSSION OF QUALITY OF CARE
In fulfilling a physician shortage gap, the question of whether the quality of care rendered by NPs and PAs is comparable to physician care is often discussed. As of 2020, four randomized controlled trials have been undertaken with NPs, and all four found that they can substitute for primary care physicians in US medicine. Work undertaken by health services researchers at Duke University showed that outcomes of care involving medically complex patients in the Veterans Health Administration (“VHA”) are the same whether the medical provider was a PA, NP, or physician.[4] NPs and PAs can manage complex patients not only cost effectively but efficiently, safely, and adequately substituting for primary care physicians depending on the situation.
![]() INCREASED ACCESSIBILITY
INCREASED ACCESSIBILITY
With ever increasing physician salaries, healthcare providers are often faced with the possibility that care rendered to the underinsured population (e.g., those covered under Medicaid) will not yield financially viable outcomes. Exacerbating this issue, in response to the COVID-19 Pandemic, the federal government introduced measures to improve access to public and private health insurance. For example, the Families First Coronavirus Response Act (“FFCRA”) required states to provide continuous coverage for Medicaid beneficiaries for the duration of the COVID-19 public health emergency.[5] In 2021, 36.8 percent of people in the US were covered through public health insurance.[6]
According to a study in Health Care Management Review, among primary care and single medical subspecialty practices employing NPs and PAs, there was an increase in the likelihood of accepting Medicaid patients.[7] Another study demonstrated greater appointment availability for new Medicaid beneficiaries among primary care practices with NPs and/or PAs and is consistent with the proposition that healthcare providers may hire NPs and PAs as a means to offer lower cost services to accommodate Medicaid patients.[8] In this situation, the utility of NPs versus PAs would appear to be on par.
![]() CONCLUSION
CONCLUSION
As the looming physician shortage materializes, organizations will need to find ways to fill the gap in the healthcare needs of their patients. One solution is through the hiring and contracting of NPs and PAs.[9] Although a lower cost solution to physician engagement, increased demand of NPs and PAs will naturally drive an increase in both the competitiveness of hiring, and compensation payable to, such providers, which, in turn, may lead to greater regulatory scrutiny of such arrangements. Healthcare organizations are encouraged to speak with a valuation expert who is familiar with healthcare regulations and compensation trends when negotiating compensation for NPs and PAs in this increasingly competitive market.
[1] https://www.aamc.org/news-insights/us-physician-shortage-growing
[2] It is worth mentioning that the previous nomenclature for a Physician Associate was a “Physician Assistant.” However, as the shift of “PA” nomenclature occurs, the privileges and scope of practice associated with the profession remains unchanged; that is, generally, a PA’s scope of practice continues to be determined by state law.
[3] Glass, K. (2022, December 16). Nurse Practitioner vs. Physician Assistant: Key Differences. University of St. Augustine for Health Sciences. https://www.usa.edu/blog/np-vs-pa/
[4] Hooker, R. (2020). Can PAs and NPs manage complex patients?. Journal of the American Academy of Physician Assistants, 33 (8), 53-54. doi: 10.1097/01.JAA.0000684140.98683.92.
[5] https://www.census.gov/content/dam/Census/library/publications/2022/acs/acsbr-013.pdf
[6] Id.
[7] Barnes, H. , Richards, M. , Martsolf, G. , Nikpay, S. & McHugh, M. (2022). Association between physician practice Medicaid acceptance and employing nurse practitioners and physician assistants. Health Care Management Review, 47 (1), 21-27. doi: 10.1097/HMR.0000000000000291.
[8] Barnes, H. , Richards, M. , Martsolf, G. , Nikpay, S. & McHugh, M. (2022). Association between physician practice Medicaid acceptance and employing nurse practitioners and physician assistants. Health Care Management Review, 47 (1), 21-27. doi: 10.1097/HMR.0000000000000291.
[9] Barnes, H. , Richards, M. , Martsolf, G. , Nikpay, S. & McHugh, M. (2022). Association between physician practice Medicaid acceptance and employing nurse practitioners and physician
