Originally published in the American Association of Provider Compensation Professionals Bulletin on August 1, 2023.
![]() OVERVIEW
OVERVIEW
The use of healthcare provider compensation data (generically referred to herein as the “Surveys”) is common practice amongst both operators and valuators, and, although widely utilized, is susceptible to misinterpretation and/or misapplication. As a prime example, the Surveys, which include those published by Medical Group Management Association (“MGMA”) and American Medical Group Association (“AMGA”), make it clear that reported data (e.g., total cash compensation, professional collections, work relative value units (“wRVUs”), etc.) correspond to “full-time” providers. But what does it mean to be a “full-time” provider, and why is that important? This article explores the various ways in which a full-time equivalent (“FTE”) is defined, and the role that such definition has in evaluating, analyzing, and utilizing data from the Surveys.
![]() DEFINITION OF AN FTE
DEFINITION OF AN FTE
An FTE is meant to standardize the concept of a full-time provider; however, even amongst the Surveys, there are various definitions of FTE, with certain Surveys failing to clearly define FTE altogether.
Broadly speaking, the existing definitions of FTE are vague, and tend to defer to each particular organization’s “normal” workweek or minimum weekly work requirements. By way of example, MGMA cites two examples within its definition of “Clinical FTE,” including two physicians both working 32 clinical hours per week as either a (i) 1.0 FTE, or (ii) 0.64 FTE, dependent upon what constitutes a “normal” workweek for the provider within a particular organization. The applicable text from MGMA is restated below.[1]
Clinical Full Time Equivalent (FTE) Also referred to as: cFTE
A measure based upon the number of hours worked on clinical activities for each provider. A provider cannot be more than 1.0 FTE but may be less. For example, a physician administrator who is 80 percent clinical and 20 percent administrative would be 0.8 clinical FTE; a physician with a normal workweek of 32 hours (4 days) working in a clinic or hospital for 32 hours would be a 1.0 clinical FTE; a physician with a normal workweek of 50 hours (5 days) working 32 clinical or hospital hours would be a 0.64 clinical FTE (32 divided by 50 hours).
Certain Surveys include supplemental data that may provide additional insight into what constitutes a typical full-time workload, as represented in such Survey. For example, AMGA reports required clinical hours per week for full-time providers. Additionally, MGMA includes annual hours of: (i) vacation, (ii) sick time, and (iii) total paid time off (inclusive of vacation, sick, and personal days) separated by physician specialty, each of which could be used as a means of estimating actual workdays per year. It is important to note, however, that reporting such data is not required for survey participants, and therefore, the number of respondents tends to be lower than other primary reporting metrics, such as cash compensation and measures of productivity.
Having shown that the definition of FTE is not uniform and generally open to some aspect of interpretation by both Survey respondents and end users, it is imperative to develop a “best” practice when interpreting and referencing Survey data as demonstrated by the following case studies.
![]() CASE STUDY ONE: CONSISTENCY IN FTE DETERMINATION
CASE STUDY ONE: CONSISTENCY IN FTE DETERMINATION
As mentioned above, the Surveys include various metrics that may be utilized in order to derive the hours associated with an FTE. As the following Tables 1 and 2 demonstrate, such data is open to interpretation, which can yield drastically different compensation outcomes for our hypothetical physicians, Dr. A and Dr. B, who perform similar services:
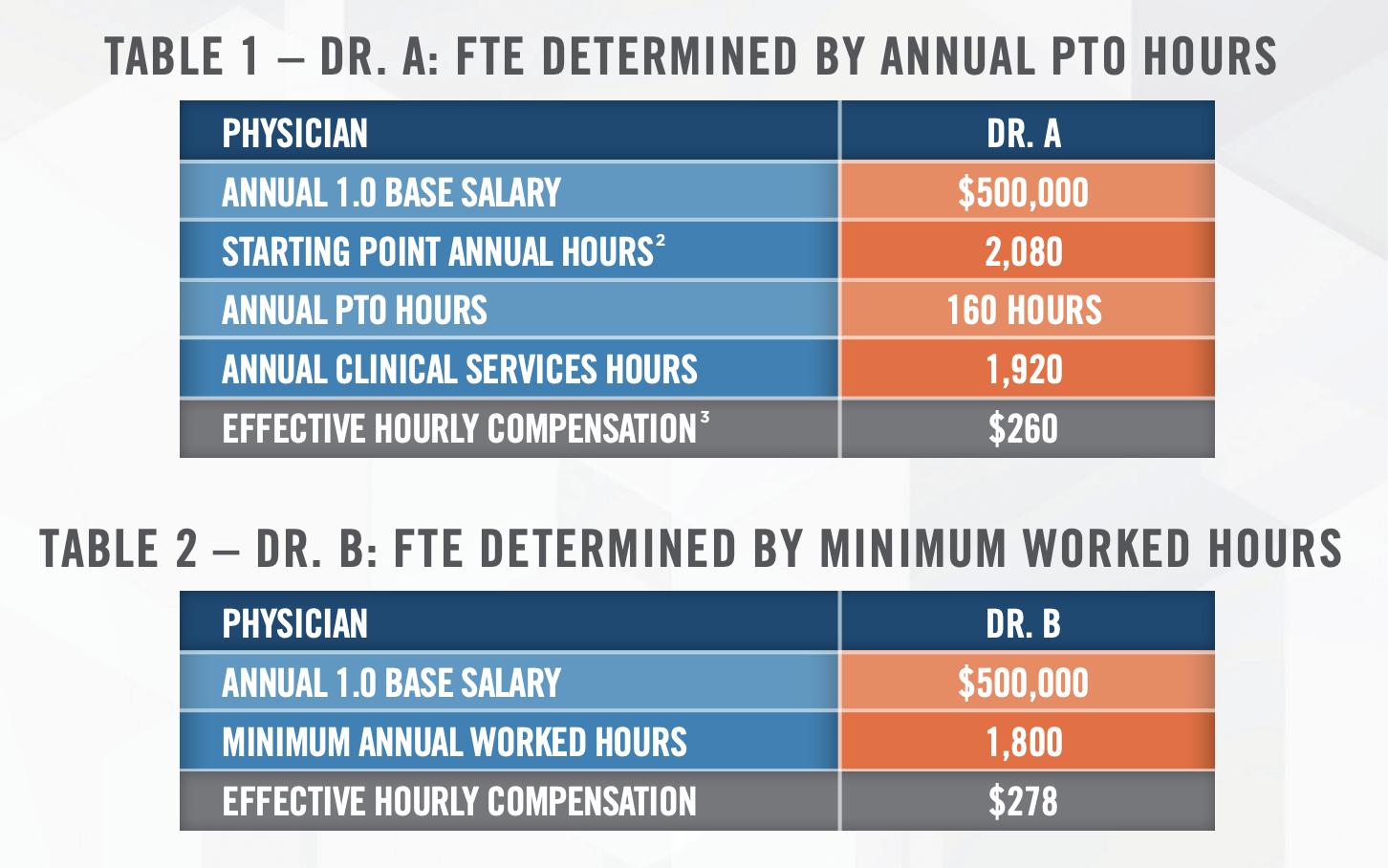
While consistency in application of a methodology to define FTE should be best practice by organizations, to the extent different methodologies are utilized for deriving FTE across specialties and/or providers, it is important to document your support and reasoning for such application.
![]() CASE STUDY TWO: DETERMINING FTE – WEEKLY CLINICAL SERVICES HOURS
CASE STUDY TWO: DETERMINING FTE – WEEKLY CLINICAL SERVICES HOURS
According to the American Medical Association, most physicians work between 40 and 60 hours each week.[4] If a physician is compensated based purely on productivity or actual worked hours, the required hours of clinical services per week is not necessarily relevant, since the physician’s compensation is ultimately tied back to the actual work effort.[5] However, if a physician is compensated based on an annual salary, it is reasonable to expect compensation differences between a physician who provides 40 hours per week versus a physician who provides 52 hours per week in the same type of role. By way of example, Dr. A and Dr. B are employed by the same organization to perform similar roles. These physicians only provide clinical services under their hypothetical agreements, as detailed in Table 3, below:
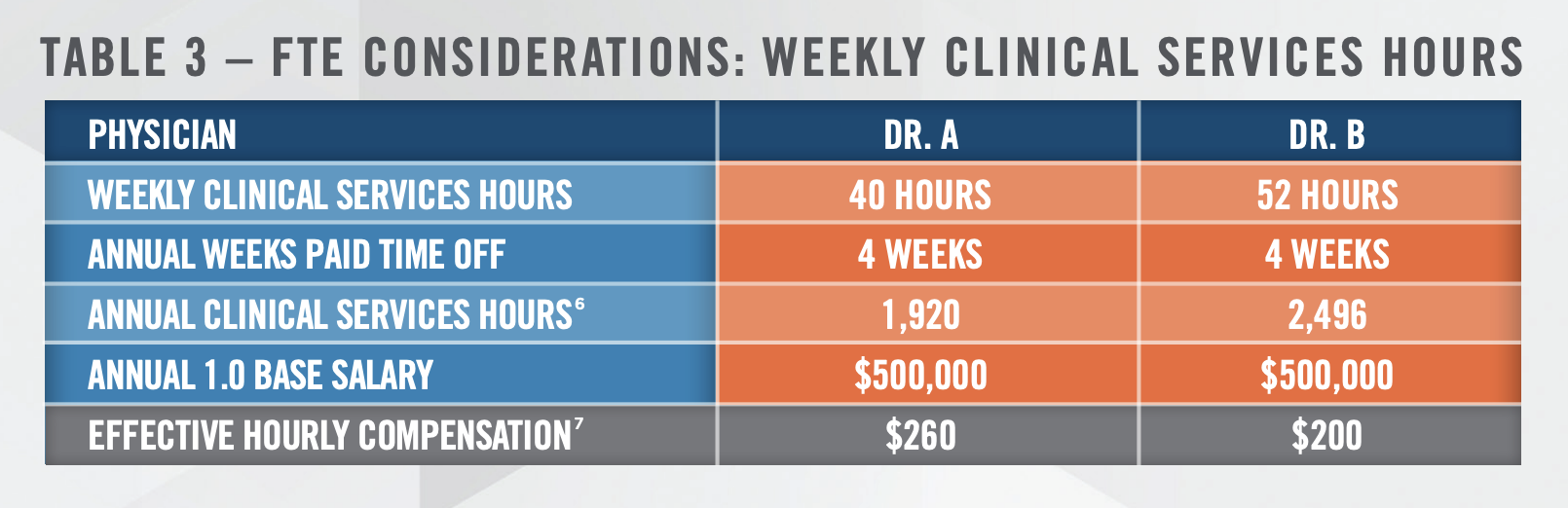
Relying on MGMA’s definition of FTE, each of these physicians would be considered a 1.0 clinical FTE; however, when utilizing Survey data to derive a guaranteed salary, is it inappropriate for both Drs. A and B to receive the same annual salary? Maybe. If both physicians historically have produced at comparable levels as measured by work relative value units or some other metric, a similar annual salary may be appropriate. Alternatively, if both physicians are inexperienced new hires and have comparable backgrounds, training, and certification, an argument could be made that Dr. B should receive a higher annual salary than Dr. A. specifically considering that Dr. B would be required to perform 30% more hours each week than Dr. A.
Bringing this discussion point full circle is the fact that both physicians responding to a particular Survey would report the same total compensation with significantly different required work hours. However, as the data is aggregated amongst all Survey participants, end users would not be able to identify such differences, thus reiterating the importance of careful and prudent analyzation and application of Survey data.
![]() CASE STUDY THREE: PAID TIME OFF AND FTE
CASE STUDY THREE: PAID TIME OFF AND FTE
In our final example in Table 4, Dr. A and Dr. B are entitled to drastically different annual weeks of paid time off.
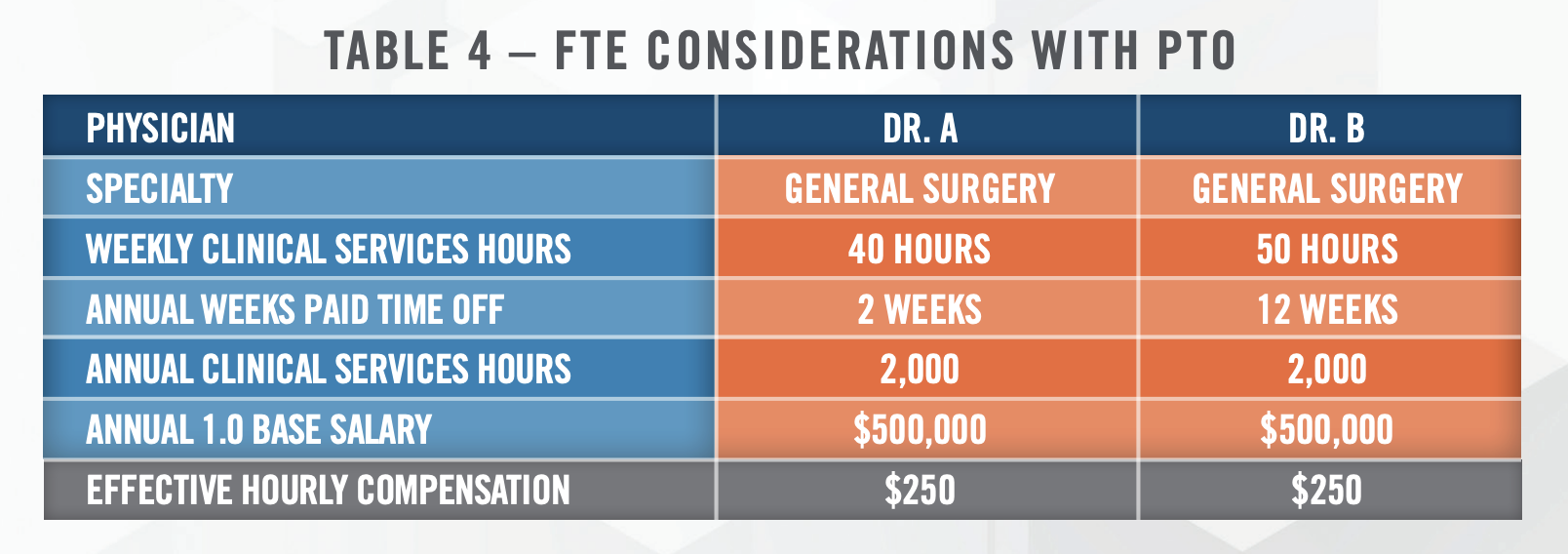
Referring to Table 4, although Dr. B is entitled to 10 more weeks of PTO than Dr. A, total annual hours worked by Dr. B are the same as those for Dr. A, as Dr. B is required to provide 50 weekly work hours versus 40 weekly work hours for Dr. A. This observation highlights the importance of looking at multiple reference points in determining a particular provider’s FTE status. It is also important to note that certain shift-based specialties and/or production-based compensation structures do not typically include any paid time off. Therefore, in situations in which such providers are offered paid time off, even if consistent with what is offered to similarly situated providers within the organization, it is necessary to determine if the benchmark survey data reflects a somewhat comparable work requirement.
![]() CONCLUSION
CONCLUSION
This article explored the definition of FTE as one of many ways that Survey data is susceptible to misinterpretation and/or misapplication. As always, when using Survey data, it is important to understand what is included in such data and to make adjustments, as necessary. As such, when utilizing Survey data for provider compensation purposes, it is essential to: (i) develop and follow best practices, (ii) establish consistent approaches to application, and (iii) document any deviations to such approaches.
[1] MGMA Datadive Provider Compensation and Production Glossary. MGMA DataDive Provider Compensation and Production Glossary; Last accessed July 26, 2023.
[2] Calculated as 40 hours per week x 52 weeks per year.
[3] Calculated as 1.0 FTE Compensation / Minimum Work Requirement
[4] American Medical Association. How many hours are in the average physician workweek? January 6, 2015. https://www.ama-assn.org/practicemanagement/physician-health/how-many-hours-are-average-physician-workweek. Last accessed July 26, 2023.
[5] One exception being inconsistent determination of FTE for purposes of deriving an hourly rate of compensation to be applied to such worked
hours, as demonstrated supra.
[6] Calculated as Weekly Clinical Services Hours x 48 worked weeks (52 annual weeks – 4 weeks PTO).
[7] Calculated as Annual Base Salary / Annual Clinical Services Hours

