As hospitals and health systems grapple with the challenges of increasing costs, regulatory uncertainty, expanding competition, and value-based payment models that require improvement in both quality and outcomes, hospital/physician alignment strategies continue to be of paramount importance. The recent spate of consolidations among large healthcare systems appears to be driven by several forces, including the anticipated value inherent in improved economies of scale and reduced competition, as well as expanded access to services. Furthermore, the entry of private equity in the healthcare services market signals that investors believe there is money to be made within the healthcare economy. Initially, private equity focused on the acquisition of companies providing products and services to the healthcare sector. However, in light of the recent $5.6 billion acquisition of LifePoint Health by Apollo Global Management, it appears that investors are betting that the provider market will generate profits through selective market expansion, greater leverage in dealing with payers, and cost containment. The impact of these changes on physicians and patients is yet to be determined.
Notwithstanding the myriad of forces being exerted to restructure and refine the healthcare industry, the development of effective structures to engage physicians as bona fide contributors to the success of the enterprise remains of fundamental importance. To achieve desired operational results, hospitals/health systems must implement structures to engage and reward physicians for their contributions to the achievement of hospital-defined goals and objectives. Alignment between hospitals and physicians, including both specialists and primary care providers, should be considered a fundamental building block for the achievement of operational and fiscal success.
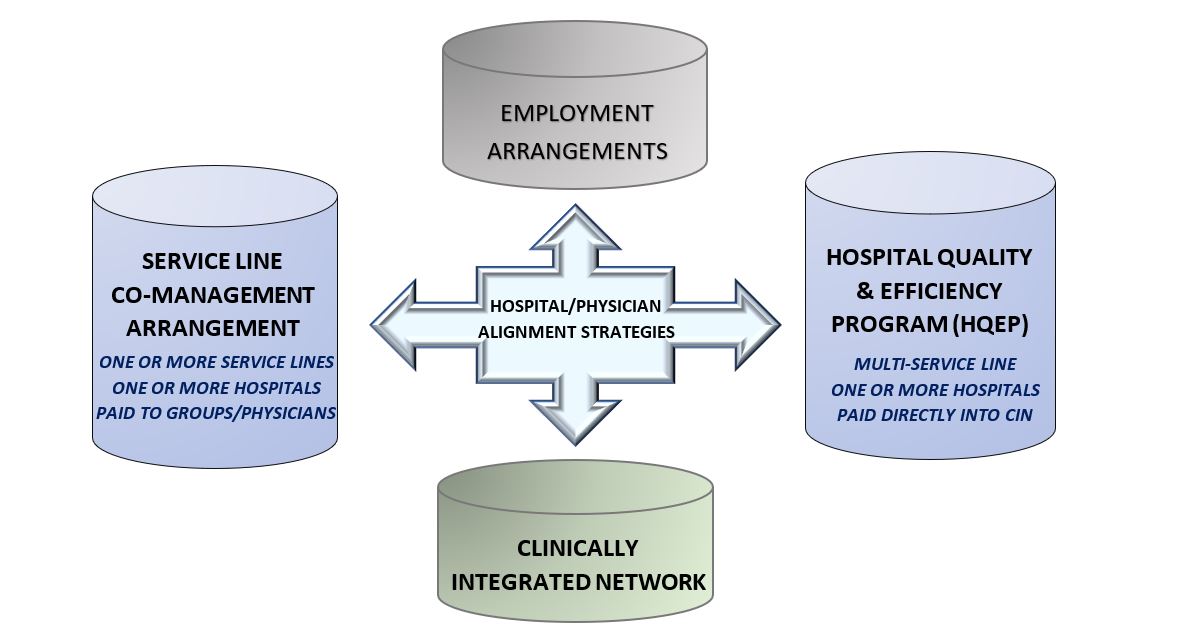
Hospital/physician alignment strategies can take many forms, ranging from the employment of physicians to the engagement of physicians in various structures that provide rewards for the achievement of performance improvement on measures involving quality, efficiency and cost effectiveness. These performance-based arrangements can accommodate both employed physicians and independent contractors. Further along the alignment continuum is the clinically integrated network, which can serve as a more comprehensive and overarching vehicle for hospital/physician alignment.
Alignment Across a Single Service Line
Predicated on the belief that shared responsibility and common goals will result in quality improvement and operational efficiencies, the ‘co-management arrangement’ is a popular vehicle for establishing hospital/physician alignment on a single service line basis as a means of facilitating the achievement of service line goals and objectives. These single service line arrangements, which can be structured to encompass the continuum of care across one or more hospitals, have proven to be excellent in facilitating the achievement of shared goals at a single service line level (e.g., orthopedic services, cardiovascular services, neurosciences, etc.). In addition to offering significant benefits to the hospital, these single service line arrangements are not difficult to implement and can serve as a first step in establishing more comprehensive alignment strategies.
Alignment Across Multiple Service Lines
One of the challenges inherent in newly-emerging, performance-based payment systems involves the reality that service lines must often work cooperatively across the enterprise to achieve the desired results. In other words, the achievement of enterprise-wide operational goals generally requires that multiple service lines work together to facilitate the attainment of hospital-/system-wide objectives. Other than the possibility of implementing similar performance improvement goals and objectives, single service line arrangements have limited ability to impact the more extensive hospital-/system-wide objectives required by value-based payment systems. As a result, there has been a trend toward expansion of single service line arrangements into more comprehensive multiple service line arrangements, which can span the continuum of care across one or more hospitals. These types of arrangements are often referred to as hospital quality and efficiency programs or HQEPs.
In Conclusion
Other than differences in the scope of services considered, a single service line co-management arrangement, and the broader multi-service line HQEP arrangement, have a significant number of similarities. Both are based on two components: (i) performance of certain pre-identified fixed duties, and (ii) achievement of identified performance-based objectives. Within the framework of a single service line arrangement, all the performance-based objectives are related to the identified service line (e.g., all metrics relate to orthopedic surgery services within an orthopedic surgery service line arrangement). However, since HQEPs are much broader in scope and include multiple service lines across one or more hospitals, performance-based objectives can have a significant impact on the achievement of value-based payment requirements, including hospital- or system-wide reduction in infection rates and readmission rates, and improvements in quality and patient satisfaction. In addition, performance-based objectives can address cost containment issues such as supply standardization, effective utilization of available resources, and transitions in care.
