Author: Scott M. Safriet
Hospital/physician alignment strategies are increasing in popularity as government and private sector payors transition to performance-based payment systems. In preparation for the continuing shift to payment structures that focus on clinical outcomes and best practices, Hospitals have been considering a diverse array of operational and structural options. Today, and in the foreseeable future, success will be very much contingent on how well healthcare providers and delivery systems implement measures to achieve required operational efficiencies, while simultaneously adapting to payment structures that link compensation to measurable improvements in quality and clinical outcomes.
As a result, hospitals and health systems are struggling with a myriad of issues including, the development of effective structures to engage physicians as bona fide contributors to the operational changes required to improve quality and efficiency, as mandated by the new payment systems. In fact, when evaluating the impact of the new healthcare payment systems on the future success of hospitals and health systems, consideration must be given to the level of physician involvement in collaborating with the hospital/health system to achieve required quality and efficiency goals.
THE CO-MANAGEMENT ARRANGEMENT
Predicated on the belief shared responsibility and common goals will result in quality and operational efficiencies, the service line co-management arrangement continues to be a popular vehicle for facilitating working partnerships between hospitals and their physicians. Notwithstanding, the service line co-management arrangement has received some criticism for its singular focus on a specific service line (e.g., cardiovascular, orthopedic surgery, neuroscience, etc.). However, when managed properly, these arrangements have consistently demonstrated that hospital/physician partnerships, based on shared goals, can result in operational efficiency and quality improvement across a hospital-based service line.
However, one of the challenges inherent in the newly developing performance-based payment systems involves the reality that service lines must work cooperatively across the enterprise in order to achieve the desired results. In other words, the achievement of enterprise-wide operational goals will require often disparate service lines to work together for the attainment of common objectives. Other than sharing similar performance improvement metrics/objectives, traditional service line co-management arrangements have limited ability to impact operations across the enterprise.
THE HOSPITAL QUALITY AND EFFICIENCY PROGRAM
New payment systems will fundamentally change the healthcare delivery system by mandating better care and improved outcomes at a lower cost on both an inpatient and outpatient basis across the continuum of care. Shared savings programs will continue to reimburse providers for meeting target spending levels on a population wide basis; thereby, incentivizing the best quality care in the most cost effective location, and potentially shifting at least some care from more expensive inpatient settings to potentially less costly outpatient settings. Identified operational and quality goals must be accomplished while simultaneously dealing with the rising costs of drugs, the need for newer and more expensive technologies and the potential reduction of reimbursement for inpatient care.

Value based purchasing and shared savings programs will exert significant pressure on Hospitals to meet operational and quality targets or face significant financial penalties. For example, under the Hospital Value Based Purchasing Program, Medicare reduced payment rates to all hospitals this year by 1.25%, while setting aside $1.1 billion for performance – based incentives. While every hospital is getting some amount of money back, data indicate that this year more than 50% of hospitals will not recoup the 1.25% in payments they initially forfeited; thus, making them net losers. Furthermore, the disparity in payments between hospitals that achieve the desired results, and those that do not, will become even more significant as the percentage of money at risk is set to grow by 0.25% per year. In addition, next year readmission penalties grow to 3 percent, and another performance–based program will be initiated that takes an additional 1% of payments away from those hospitals with the highest percentage of patients who suffered injury or infection during an inpatient stay[1]
Therefore, an environment which fosters successful collaboration between the hospital/health system and its physicians to focus on both quality and cost effectiveness is of paramount importance. In fact, it may arguably be considered as the most critical component of success in navigating the impact of the changing health care environment on a hospital’s or health system’s bottom line. As a result, there has been a trend toward expansion of the single service line co-management arrangement into a more comprehensive hospital or system-wide arrangement, which incorporates multiple service lines across one or more hospitals. These types of arrangements, which are often referred to as hospital efficiency programs (“HEPs”) or hospital quality & efficiency programs (“HQEPs”), may also be thought of as a hospital/system-wide, multi-service line co-management arrangements.
Other than scope of services considered, the service line management arrangement and the broader HEP or HQEP arrangements, have a significant number of similarities. Both are based on two component parts: (i) the performance of certain pre-identified fixed tasks, which address daily operational requirements; and (ii) performance-based incentives, which require the achievement of specific objectives and performance thresholds for compensation to be paid. Within the framework of a single service line co-management arrangement, all the performance-based metrics are focused on the identified service line (e.g., all metrics relate to orthopedic surgery). However, since HEPs are much broader in scope and generally include multiple service lines across the hospital or enterprise, performance-based metrics requiring collaboration and cooperation across multiple service lines can also be incorporated into the arrangement to facilitate the achievement of hospital-wide goals and objectives (e.g., reduction in hospital acquired infection rates, reduction in readmission rates, or reduction in cost per case by some fixed percentage across the hospital, and/or the achievement of 100% on all SCIP measures as applied to all surgical patients across the entire hospital or health system, etc.).
Due to differences in scale, the FMV of compensation available within a HEP arrangement is often significantly higher than in a service line co-management arrangement. It is also assumed that the coordination of activities required to achieve hospital/system-wide performance objectives across multiple service lines will require a high level of collaboration and joint work effort among all physicians. The result, however, offers the opportunity for exponentially higher quality improvement and operational efficiencies than can be achieved in a traditional service line co-management arrangement.
THE CLINICALLY INTEGRATED NETWORK
As mentioned previously, the transition to value-based reimbursement systems by federal government and commercial payers will ultimately result in an expanding emphasis on cost effectiveness and improved outcomes across the hospital or health system as a whole. These new payment systems will fundamentally change the healthcare delivery system by mandating better care at a lower cost. As a result, there will be significant pressure exerted on hospitals and health systems to meet operational and quality targets, or face financial penalties and lower reimbursement rates.
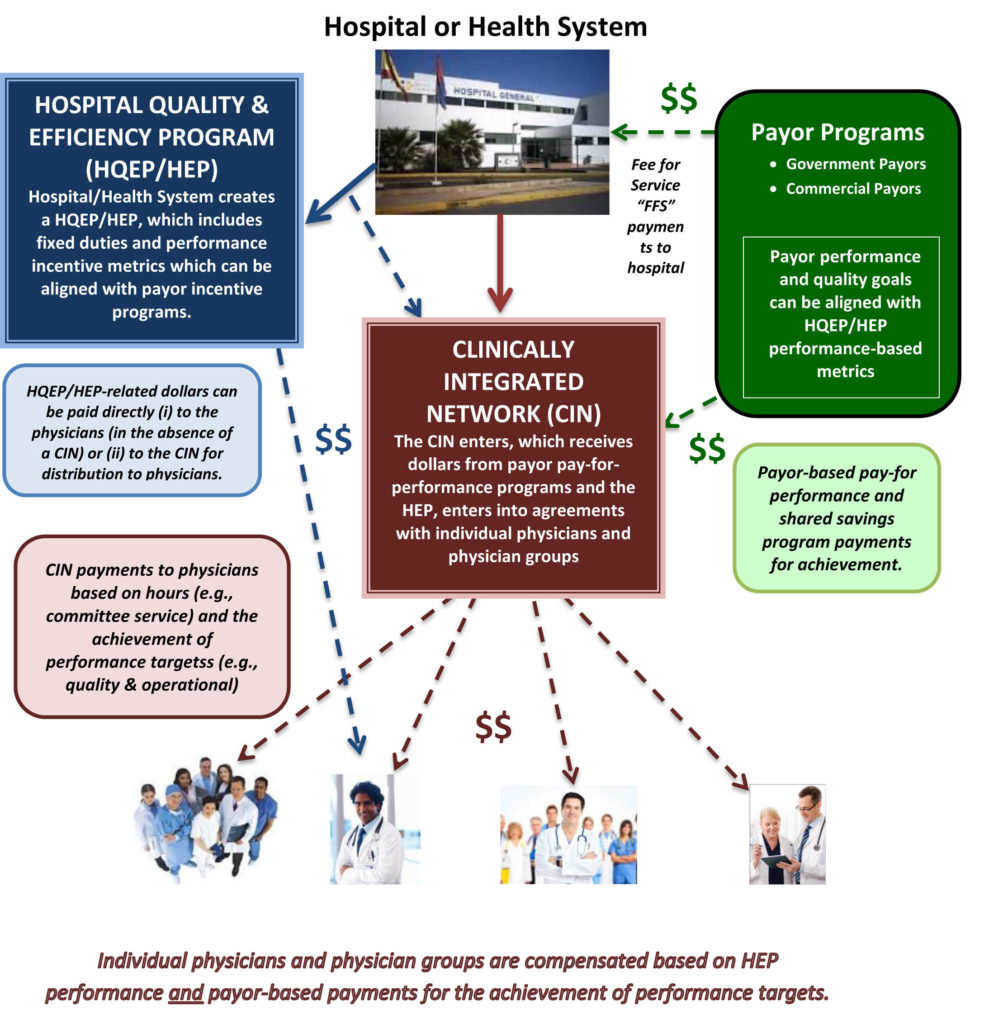
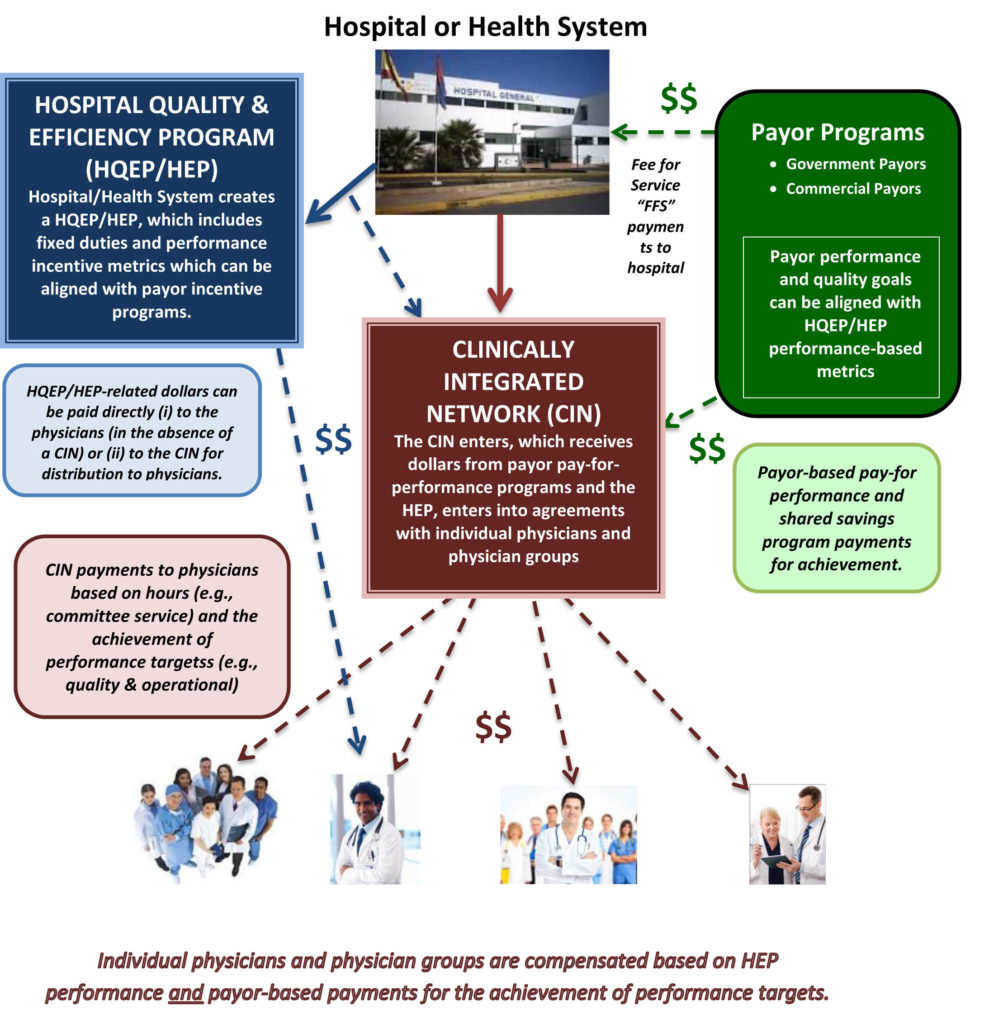
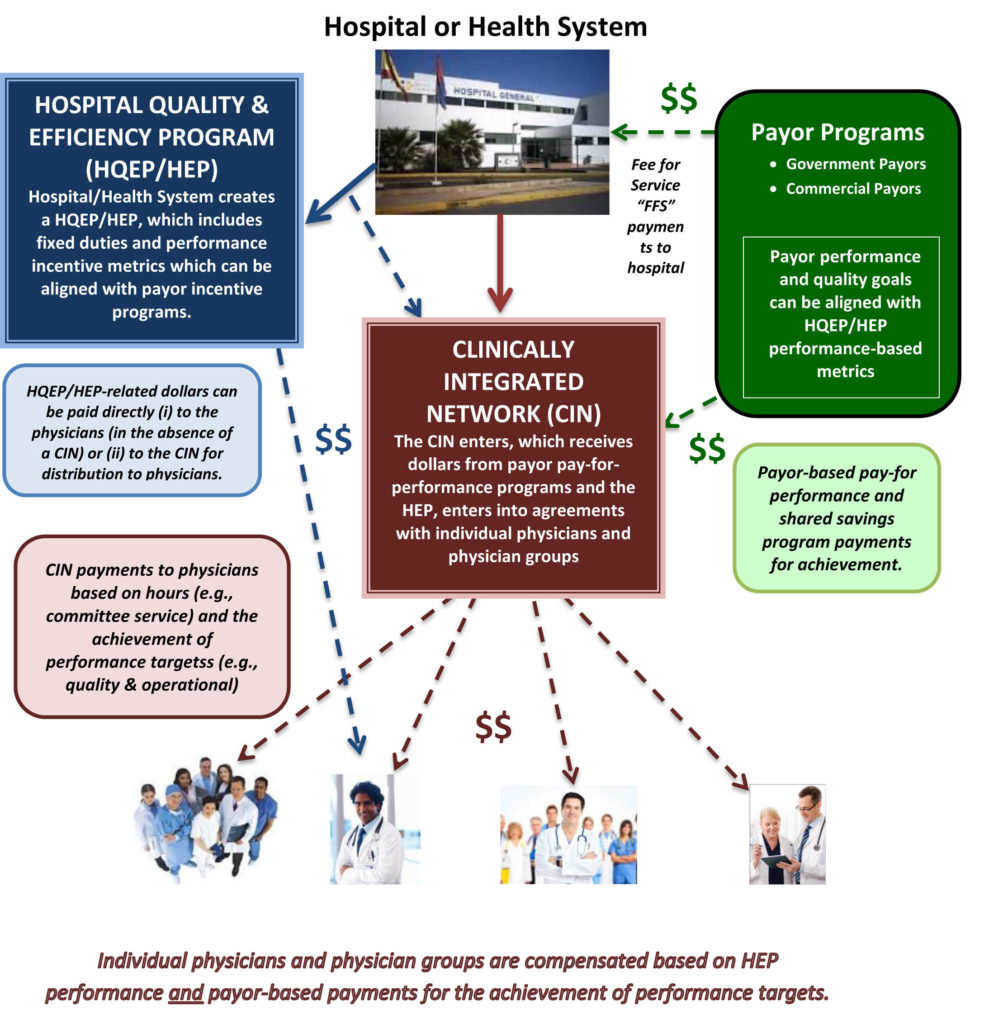
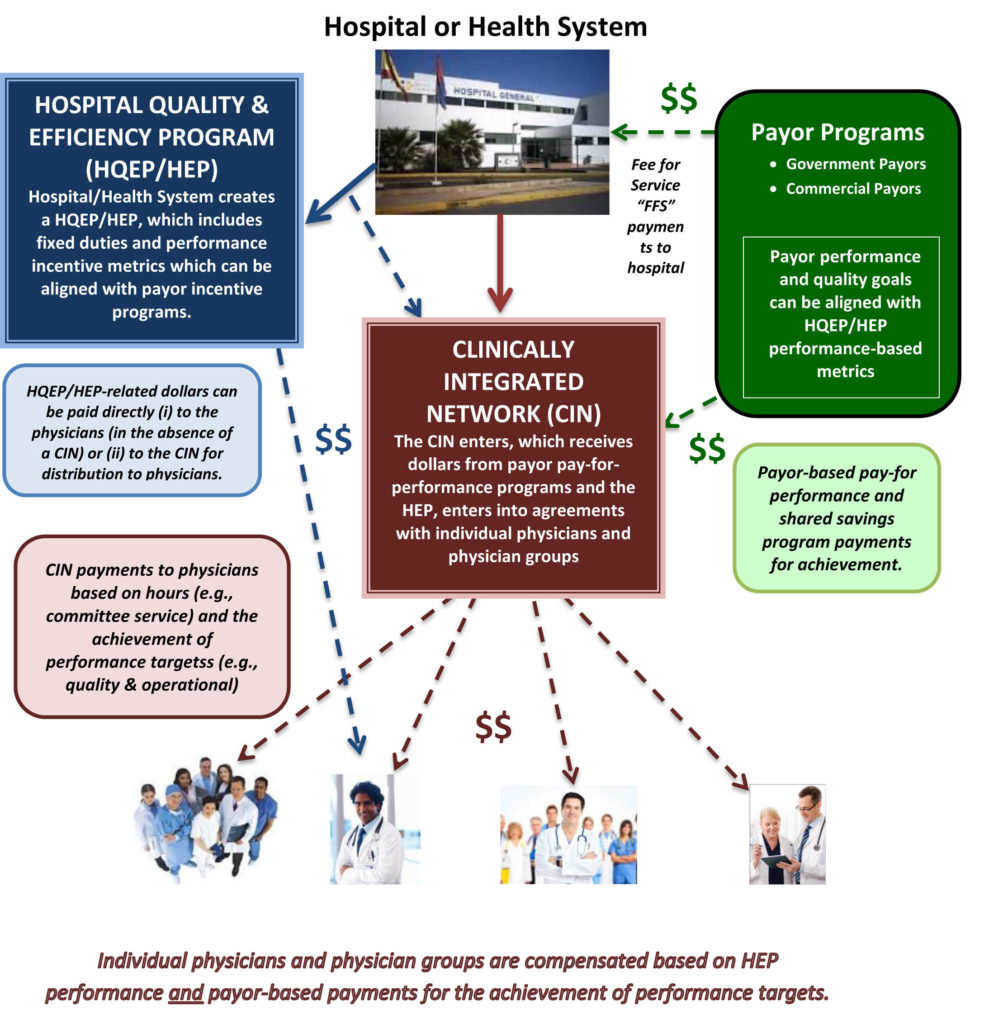
The clinically integrated network or “CIN” brings together the hospital, physicians and other healthcare providers to deliver services focused on quality, performance and efficiency. The CIN, through its providers, typically involves a variety of activities, including (i) coordination of the continuum of care through affiliated providers and facilities in order to improve the quality and access to care; (ii) development and implementation of evidence-based protocols and guidelines to improve outcomes; (iii) performance improvement, increased operational efficiency and overall cost-savings; and (iv) collective contracting with payors based on contractual arrangements that drive clinical and operational improvement.
If structured properly, the CIN offers the advantages of a HEP/HQEP, while adding significant benefits associated with linking pay for performance programs including, shared savings and value-based payment programs into the compensation mix. In other words, the CIN can receive funds from a variety of sources, including hospital or system-wide HEP/HQEP arrangement as well as payor initiated performance-based programs. The incorporation of the HEP/HQEP with the CIN serves the hospital’s and/or health system’s goals of achieving desired quality and efficiency goals, while adding financial benefits associated with attracting third party payor programs, including pay-for-performance and value-based payment programs, into the compensation mix. As a result, the CIN can receive funds from a variety of sources to incentivize the achievement of quality and operational targets.
Co-management arrangements, HEPs/HQEPs and CINs all share a common focus on collaboration between the hospital/health system and its clinical providers as the primary mechanism for the achievement of measurable results and improved outcomes. Therefore, expanding the scope of an arrangement from a single service line to a hospital or system-wide program, offers greater opportunities for improved operational efficiencies, cost savings and quality improvements.
Since the development and operation of shared savings and value-based payment programs is often a long and arduous project, many hospitals and health systems have not yet fully implemented these types of programs. However, the need for a viable mechanism to facilitate hospital-physician alignment may be required relatively quickly, as success within the new payment models will require that physicians and hospitals work together to achieve identified goals and objectives. Therefore, it is not unreasonable to consider a multi-phase approach for introducing alignment opportunities across the hospital/system.
The overarching goal of each of these arrangements is to (i) involve a larger number of medical staff physicians in processes required to improve outcomes and reduce costs and (ii) encourage the achievement of identified goals and objectives through incentive-based compensation. The form of these arrangements can vary significantly based upon the specific circumstances, needs, and objectives of the hospital/system. For example, new or existing service line co-management arrangements can be established or expanded across one or more hospitals within a system. This can be accomplished through the implementation of multiple service line co-management arrangements (e.g., cardiovascular, orthopedic, surgical services, neuroscience, gastroenterology, women’s services, hematology/oncology, primary care, pain management, etc.). , or through the creation of a HQEP/HEP, which can serve as a hospital-wide multi-service line co-management arrangement. Once implemented, the HQEP/HEP can be easily incorporated into a CIN.
The Determination of Fair Market Value: Evolving Issues
The increasing popularity of co-management, HQEP/HEP and CIN arrangements, coupled with the unique dynamics of each individual hospital and health system, has led to significant variation in their structure and application. Therefore, the structure of the arrangement will serve as the primary driver in determining the most appropriate valuation approach to use in calculating the fair market value (“FMV”) of the arrangement.
Typically, HEP/HQEP arrangements include the following:
- A fixed Base Fee (paid monthly, quarterly, semi-annually or annually), that provides compensation for the time required to coordinate, oversee and manage the multi-service line quality and efficiency programs included in the HEP/HQEP. Often, payment of the Base Fee is based on actual physician time (tracked and documented) spent serving on hospital/health system committees related to operational, quality and efficiency improvement.
- A variable Incentive Fee (paid quarterly, semi-annually or annually), paid for meeting certain pre-determined operational, quality and efficiency targets. Dollars associated with the Incentive Fee are 100% at risk, and will not be paid unless some pre-established level of performance improvement is achieved.
Among the factors to consider when implementing a HEP/HQEP, are those related to the performance improvement metrics and their commercial reasonableness. For example, as performance-based measurers, they must be capable of demonstrating measureable performance improvement. Therefore, existing or current-state baseline performance, for each included performance improvement measure, must be identified prior to establishing payment targets/thresholds, in order to assure that they will be paid based on actual performance improvement.
There are many other considerations when developing and implementing performance improvement measures. However, a complete discussion of all of the factors to consider would be beyond the scope of this paper. Notwithstanding, the following represents a summary of some of the most important elements to consider when developing performance improvement measures in the context of HEP/HQEP arrangements:
- Performance improvement incentives should reward for demonstrated “improvement” over current or “baseline” performance. In other words, payment for a particular incentive measure is achieved only if the baseline performance is exceeded;
- If the performance measure does not reward for improvement but rather, rewards for “maintaining” baseline performance, then the baseline performance must be at “national standard” levels. To that end, the source of the standard (e., Press Ganey, STS, CMS) as well as the national standard level should be appropriately documented;
- There must be a sufficient number of included measures;
- Performance metrics should not relate to any activity which could be perceived as generating patient referrals.
- There must be, at minimum, a six-month measurement period (e.g., development of an operational protocol or procedure for six-months, and measurement of compliance operational improvement for six moths).
- “New Program Development” incentive metrics may be included when opportunities exist for the establishment of new programs, locations or certifications. For example,
- Center of Excellence Designation; or
- Development of new service lines or locations.
In general, New Program Development incentive metrics should include very specific milestone activities and dates that must be reached to receive payment. Furthermore, the payment amount associated with each milestone should be proportional to the amount of time required to achieve the identified milestone. For example,
- Development of a business case by xx/xx/xx date (g. if this activity will be completed by the end of Q1, then total payment for achieving this milestone should be no greater that 25% of dollars associated with the entire metric);
- Achievement of hospital/health system approval of the business case; by xx/xx/xx date; and
- Implementation of the program, service line, etc. by xx/xx/xx date.
In Summary
The emergence of new payment models for the delivery of healthcare services has contributed to the development of a broad range of continually evolving opportunities for hospital/health system-physician partnerships. The service line co-management arrangement continues to be a popular vehicle for facilitating working partnerships between hospitals and their physicians. However, due to its focus on a single service line (e.g., orthopedics, cardiovascular services, etc.), another, more comprehensive arrangement structure is gaining in popularity. The HQEP/HEP arrangement, which often includes multiple service lines across the hospital and/or health system, may be the next evolution in hospital/physician alignment structures. As they grow in popularity, these types of performance-based arrangements continue to increase in complexity, resulting in the emergence of new issues that require consideration in the valuation process.
Hospital/physician alignment strategies are increasing in popularity as government and private sector payors transition to performance-based payment systems. In preparation for the continuing shift to payment structures that focus on clinical outcomes and best practices, Hospitals have been considering a diverse array of operational and structural options. Today, and in the foreseeable future, success will be very much contingent on how well healthcare providers and delivery systems implement measures to achieve required operational efficiencies, while simultaneously adapting to payment structures that link compensation to measurable improvements in quality and clinical outcomes.
As a result, hospitals and health systems are struggling with a myriad of issues including, the development of effective structures to engage physicians as bona fide contributors to the operational changes required to improve quality and efficiency, as mandated by the new payment systems. In fact, when evaluating the impact of the new healthcare payment systems on the future success of hospitals and health systems, consideration must be given to the level of physician involvement in collaborating with the hospital/health system to achieve required quality and efficiency goals.
THE CO-MANAGEMENT ARRANGEMENT
Predicated on the belief shared responsibility and common goals will result in quality and operational efficiencies, the service line co-management arrangement continues to be a popular vehicle for facilitating working partnerships between hospitals and their physicians. Notwithstanding, the service line co-management arrangement has received some criticism for its singular focus on a specific service line (e.g., cardiovascular, orthopedic surgery, neuroscience, etc.). However, when managed properly, these arrangements have consistently demonstrated that hospital/physician partnerships, based on shared goals, can result in operational efficiency and quality improvement across a hospital-based service line.
However, one of the challenges inherent in the newly developing performance-based payment systems involves the reality that service lines must work cooperatively across the enterprise in order to achieve the desired results. In other words, the achievement of enterprise-wide operational goals will require often disparate service lines to work together for the attainment of common objectives. Other than sharing similar performance improvement metrics/objectives, traditional service line co-management arrangements have limited ability to impact operations across the enterprise.
THE HOSPITAL QUALITY AND EFFICIENCY PROGRAM
New payment systems will fundamentally change the healthcare delivery system by mandating better care and improved outcomes at a lower cost on both an inpatient and outpatient basis across the continuum of care. Shared savings programs will continue to reimburse providers for meeting target spending levels on a population wide basis; thereby, incentivizing the best quality care in the most cost effective location, and potentially shifting at least some care from more expensive inpatient settings to potentially less costly outpatient settings. Identified operational and quality goals must be accomplished while simultaneously dealing with the rising costs of drugs, the need for newer and more expensive technologies and the potential reduction of reimbursement for inpatient care.

Value based purchasing and shared savings programs will exert significant pressure on Hospitals to meet operational and quality targets or face significant financial penalties. For example, under the Hospital Value Based Purchasing Program, Medicare reduced payment rates to all hospitals this year by 1.25%, while setting aside $1.1 billion for performance – based incentives. While every hospital is getting some amount of money back, data indicate that this year more than 50% of hospitals will not recoup the 1.25% in payments they initially forfeited; thus, making them net losers. Furthermore, the disparity in payments between hospitals that achieve the desired results, and those that do not, will become even more significant as the percentage of money at risk is set to grow by 0.25% per year. In addition, next year readmission penalties grow to 3 percent, and another performance–based program will be initiated that takes an additional 1% of payments away from those hospitals with the highest percentage of patients who suffered injury or infection during an inpatient stay[1]
Therefore, an environment which fosters successful collaboration between the hospital/health system and its physicians to focus on both quality and cost effectiveness is of paramount importance. In fact, it may arguably be considered as the most critical component of success in navigating the impact of the changing health care environment on a hospital’s or health system’s bottom line. As a result, there has been a trend toward expansion of the single service line co-management arrangement into a more comprehensive hospital or system-wide arrangement, which incorporates multiple service lines across one or more hospitals. These types of arrangements, which are often referred to as hospital efficiency programs (“HEPs”) or hospital quality & efficiency programs (“HQEPs”), may also be thought of as a hospital/system-wide, multi-service line co-management arrangements.
Other than scope of services considered, the service line management arrangement and the broader HEP or HQEP arrangements, have a significant number of similarities. Both are based on two component parts: (i) the performance of certain pre-identified fixed tasks, which address daily operational requirements; and (ii) performance-based incentives, which require the achievement of specific objectives and performance thresholds for compensation to be paid. Within the framework of a single service line co-management arrangement, all the performance-based metrics are focused on the identified service line (e.g., all metrics relate to orthopedic surgery). However, since HEPs are much broader in scope and generally include multiple service lines across the hospital or enterprise, performance-based metrics requiring collaboration and cooperation across multiple service lines can also be incorporated into the arrangement to facilitate the achievement of hospital-wide goals and objectives (e.g., reduction in hospital acquired infection rates, reduction in readmission rates, or reduction in cost per case by some fixed percentage across the hospital, and/or the achievement of 100% on all SCIP measures as applied to all surgical patients across the entire hospital or health system, etc.).
Due to differences in scale, the FMV of compensation available within a HEP arrangement is often significantly higher than in a service line co-management arrangement. It is also assumed that the coordination of activities required to achieve hospital/system-wide performance objectives across multiple service lines will require a high level of collaboration and joint work effort among all physicians. The result, however, offers the opportunity for exponentially higher quality improvement and operational efficiencies than can be achieved in a traditional service line co-management arrangement.
THE CLINICALLY INTEGRATED NETWORK
As mentioned previously, the transition to value-based reimbursement systems by federal government and commercial payers will ultimately result in an expanding emphasis on cost effectiveness and improved outcomes across the hospital or health system as a whole. These new payment systems will fundamentally change the healthcare delivery system by mandating better care at a lower cost. As a result, there will be significant pressure exerted on hospitals and health systems to meet operational and quality targets, or face financial penalties and lower reimbursement rates.
The clinically integrated network or “CIN” brings together the hospital, physicians and other healthcare providers to deliver services focused on quality, performance and efficiency. The CIN, through its providers, typically involves a variety of activities, including (i) coordination of the continuum of care through affiliated providers and facilities in order to improve the quality and access to care; (ii) development and implementation of evidence-based protocols and guidelines to improve outcomes; (iii) performance improvement, increased operational efficiency and overall cost-savings; and (iv) collective contracting with payors based on contractual arrangements that drive clinical and operational improvement.
If structured properly, the CIN offers the advantages of a HEP/HQEP, while adding significant benefits associated with linking pay for performance programs including, shared savings and value-based payment programs into the compensation mix. In other words, the CIN can receive funds from a variety of sources, including hospital or system-wide HEP/HQEP arrangement as well as payor initiated performance-based programs. The incorporation of the HEP/HQEP with the CIN serves the hospital’s and/or health system’s goals of achieving desired quality and efficiency goals, while adding financial benefits associated with attracting third party payor programs, including pay-for-performance and value-based payment programs, into the compensation mix. As a result, the CIN can receive funds from a variety of sources to incentivize the achievement of quality and operational targets.
Co-management arrangements, HEPs/HQEPs and CINs all share a common focus on collaboration between the hospital/health system and its clinical providers as the primary mechanism for the achievement of measurable results and improved outcomes. Therefore, expanding the scope of an arrangement from a single service line to a hospital or system-wide program, offers greater opportunities for improved operational efficiencies, cost savings and quality improvements.
Since the development and operation of shared savings and value-based payment programs is often a long and arduous project, many hospitals and health systems have not yet fully implemented these types of programs. However, the need for a viable mechanism to facilitate hospital-physician alignment may be required relatively quickly, as success within the new payment models will require that physicians and hospitals work together to achieve identified goals and objectives. Therefore, it is not unreasonable to consider a multi-phase approach for introducing alignment opportunities across the hospital/system.
The overarching goal of each of these arrangements is to (i) involve a larger number of medical staff physicians in processes required to improve outcomes and reduce costs and (ii) encourage the achievement of identified goals and objectives through incentive-based compensation. The form of these arrangements can vary significantly based upon the specific circumstances, needs, and objectives of the hospital/system. For example, new or existing service line co-management arrangements can be established or expanded across one or more hospitals within a system. This can be accomplished through the implementation of multiple service line co-management arrangements (e.g., cardiovascular, orthopedic, surgical services, neuroscience, gastroenterology, women’s services, hematology/oncology, primary care, pain management, etc.). , or through the creation of a HQEP/HEP, which can serve as a hospital-wide multi-service line co-management arrangement. Once implemented, the HQEP/HEP can be easily incorporated into a CIN.
The Determination of Fair Market Value: Evolving Issues
The increasing popularity of co-management, HQEP/HEP and CIN arrangements, coupled with the unique dynamics of each individual hospital and health system, has led to significant variation in their structure and application. Therefore, the structure of the arrangement will serve as the primary driver in determining the most appropriate valuation approach to use in calculating the fair market value (“FMV”) of the arrangement.
Typically, HEP/HQEP arrangements include the following:
- A fixed Base Fee (paid monthly, quarterly, semi-annually or annually), that provides compensation for the time required to coordinate, oversee and manage the multi-service line quality and efficiency programs included in the HEP/HQEP. Often, payment of the Base Fee is based on actual physician time (tracked and documented) spent serving on hospital/health system committees related to operational, quality and efficiency improvement.
- A variable Incentive Fee (paid quarterly, semi-annually or annually), paid for meeting certain pre-determined operational, quality and efficiency targets. Dollars associated with the Incentive Fee are 100% at risk, and will not be paid unless some pre-established level of performance improvement is achieved.
Among the factors to consider when implementing a HEP/HQEP, are those related to the performance improvement metrics and their commercial reasonableness. For example, as performance-based measurers, they must be capable of demonstrating measureable performance improvement. Therefore, existing or current-state baseline performance, for each included performance improvement measure, must be identified prior to establishing payment targets/thresholds, in order to assure that they will be paid based on actual performance improvement.
There are many other considerations when developing and implementing performance improvement measures. However, a complete discussion of all of the factors to consider would be beyond the scope of this paper. Notwithstanding, the following represents a summary of some of the most important elements to consider when developing performance improvement measures in the context of HEP/HQEP arrangements:
- Performance improvement incentives should reward for demonstrated “improvement” over current or “baseline” performance. In other words, payment for a particular incentive measure is achieved only if the baseline performance is exceeded;
- If the performance measure does not reward for improvement but rather, rewards for “maintaining” baseline performance, then the baseline performance must be at “national standard” levels. To that end, the source of the standard (e., Press Ganey, STS, CMS) as well as the national standard level should be appropriately documented;
- There must be a sufficient number of included measures;
- Performance metrics should not relate to any activity which could be perceived as generating patient referrals.
- There must be, at minimum, a six-month measurement period (e.g., development of an operational protocol or procedure for six-months, and measurement of compliance operational improvement for six moths).
- “New Program Development” incentive metrics may be included when opportunities exist for the establishment of new programs, locations or certifications. For example,
- Center of Excellence Designation; or
- Development of new service lines or locations.
In general, New Program Development incentive metrics should include very specific milestone activities and dates that must be reached to receive payment. Furthermore, the payment amount associated with each milestone should be proportional to the amount of time required to achieve the identified milestone. For example,
- Development of a business case by xx/xx/xx date (g. if this activity will be completed by the end of Q1, then total payment for achieving this milestone should be no greater that 25% of dollars associated with the entire metric);
- Achievement of hospital/health system approval of the business case; by xx/xx/xx date; and
- Implementation of the program, service line, etc. by xx/xx/xx date.
In Summary
The emergence of new payment models for the delivery of healthcare services has contributed to the development of a broad range of continually evolving opportunities for hospital/health system-physician partnerships. The service line co-management arrangement continues to be a popular vehicle for facilitating working partnerships between hospitals and their physicians. However, due to its focus on a single service line (e.g., orthopedics, cardiovascular services, etc.), another, more comprehensive arrangement structure is gaining in popularity. The HQEP/HEP arrangement, which often includes multiple service lines across the hospital and/or health system, may be the next evolution in hospital/physician alignment structures. As they grow in popularity, these types of performance-based arrangements continue to increase in complexity, resulting in the emergence of new issues that require consideration in the valuation process.
[1] Fact sheets: CMS Final Rule to improve quality of care during hospital inpatient stays. Centers for Medicare & Medicaid Services. 8/2/13. http://www.cms.gov/newsroom/mediareleasedatabase/fact-sheets/2013-fact-sheets-items/2013-08-02-3.html
